How opioid prescriptions to Medicaid patients in Delaware stack up
This story originally appeared on Ophelia and was produced and distributed in partnership with Stacker Studio.
How opioid prescriptions to Medicaid patients in Delaware stack up
Almost 20 years after the first wave of opioid overdose deaths in the U.S., more than 75% of drug overdose fatalities were connected to opioid use in 2021, according to the latest data from the Centers for Disease Control and Prevention.
Ophelia explored how U.S. prescription opioid dispense rates in 2021 varied by state using Centers for Medicare and Medicaid Services data, which includes information about Medicaid, a public health insurance coverage for low-income households and people with certain disabilities that is offered jointly by states and the federal government.
According to the National Institute on Drug Abuse, overdose fatalities that involved opioids prescribed for pain management grew more than fivefold from 1999 to 2017, when they peaked at 17,000. Since then, the number of deaths has declined, though there was a slight increase during the COVID-19 pandemic.
Within the past decade, policies aimed at controlling the dispensing of legal opioids and promoting alternative nonopioid pain treatments have been credited for slowing the number of prescriptions and overdose deaths.
In 2021, even as most states had implemented laws regulating opioid prescription and freeing access to naloxone—opioid overdose-reversing medication like Narcan—the number of fatalities involving prescription opioids totaled 16,700.
Opioids are Schedule II controlled substances, meaning the Drug Enforcement Administration views them as narcotics with "a high potential for abuse which may lead to severe psychological or physical dependence." Though the data included here does not distinguish between the reasons for prescribing, opioids prescribed for addiction treatment—such as buprenorphine and methadone—actually work to lower the incidence of opioid overdose and lower associated deaths. Furthermore, a 2023 study in JAMA Network Open found that the COVID-era increase in methadone access for the treatment of opioid use disorder was not associated with an increase in opioid overdose deaths.
Prescription opioid overdose deaths began increasing in the 1990s when the growing circulation of oxycodone and hydrocodone led to the first wave of extensive opioid drug misuse. By 2016, opioid-related overdose deaths had reached such alarming levels that the health crisis was considered an epidemic. A year later, the U.S. government declared it a public health emergency.
Since then, 27 states passed laws regulating the duration or dosage of first-time opioid-based medication for pain treatments, statutes that resulted in a 2.23% decrease in opioid prescriptions by 2021. However, the introduction of fentanyl in the illegal drug market has delayed the fight against opioid-related overdose deaths. The CDC describes the synthetic opioid as "50 times stronger than heroin and 100 times stronger than morphine."
In Delaware, 2.8% of Medicaid claims were for opioids in 2021, or about 76,000 claims. That's a change of -5.5 percentage points since 2013, when there were 185,965 total opioid claims. Read the national analysis to see which states had the highest rates of Medicaid opioid prescriptions in 2021.
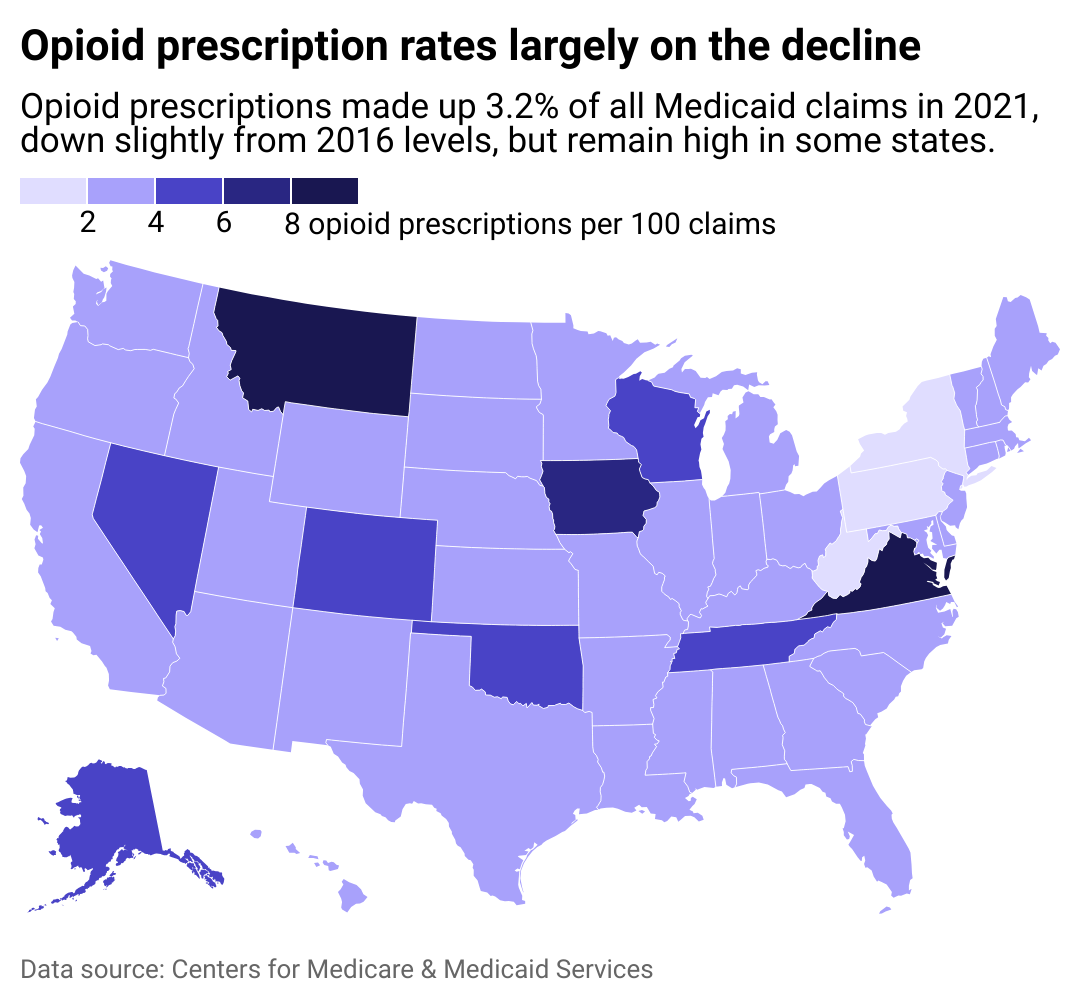
States with the highest opioid prescribing rates
Montana and Virginia had the highest number of Medicaid opioid prescriptions in 2021, followed by Iowa. Rural counties, in particular, are more affected by opioid use disorder, according to the Department of Agriculture.
At the other end of the spectrum, New York, Pennsylvania, and West Virginia have the lowest number of Medicaid opioid prescriptions. In 2015, West Virginia had the highest rate of overdose deaths in the country and one of the highest prescription rates for opioids. According to a report by the DEA, this can be attributed to the prevalence of jobs in heavy manual labor including mining, timbering, and manufacturing. Workers in these industries are prone to suffering injuries, which physicians mainly treated with opioid pain relievers.
The decrease in opioid prescriptions in West Virginia results from a statewide program designed to reduce the use of opioid-based medication after the CDC had reported a "statistically significant increase in drug overdose deaths" in 2015, according to the DEA report.
This story features data reporting by Elena Cox, writing by Martha Sandoval, and is part of a series utilizing data automation across 50 states and Washington D.C.