
Answers to 25 common COVID-19 vaccine questions
Answers to 25 common COVID-19 vaccine questions
The Food and Drug Administration (FDA) on Aug. 23 approved the Pfizer-BioNTech COVID-19 vaccine, the first full approval for a COVID-19 vaccine. Now marketed as Comirnaty, the vaccine is available for the prevention of COVID-19 disease in people 16 years and older. The vaccine is also still available under emergency use authorization for 12- to 15-year-olds, as well, and for the administering of third doses for people who are immunocompromised.
A successful vaccination campaign relies on a large enough group of people getting the vaccine in order to achieve what is known as herd immunity. While that exact number is still unknown, it is estimated that 80–90% of the population must be immune—either by vaccination or prior exposure to the virus—in order to achieve herd immunity. This means it's extremely important that people feel confident in the vaccines and vaccination process.
Stacker compiled a list of 25 common COVID-19 questions and their answers from news, scientific, and government reports.
Vaccinations for COVID-19 began being administered in the U.S. on Dec. 14, 2020. The quick rollout came a little more than a year after the virus was first identified in November 2019. The impressive speed with which vaccines were developed has also left a lot of people with a lot of questions. The questions range from the practical—how will I get vaccinated?—to the scientific—how do these vaccines even work?
Keep reading to discover answers to 25 common COVID-19 vaccine questions.
How do the different vaccines work?
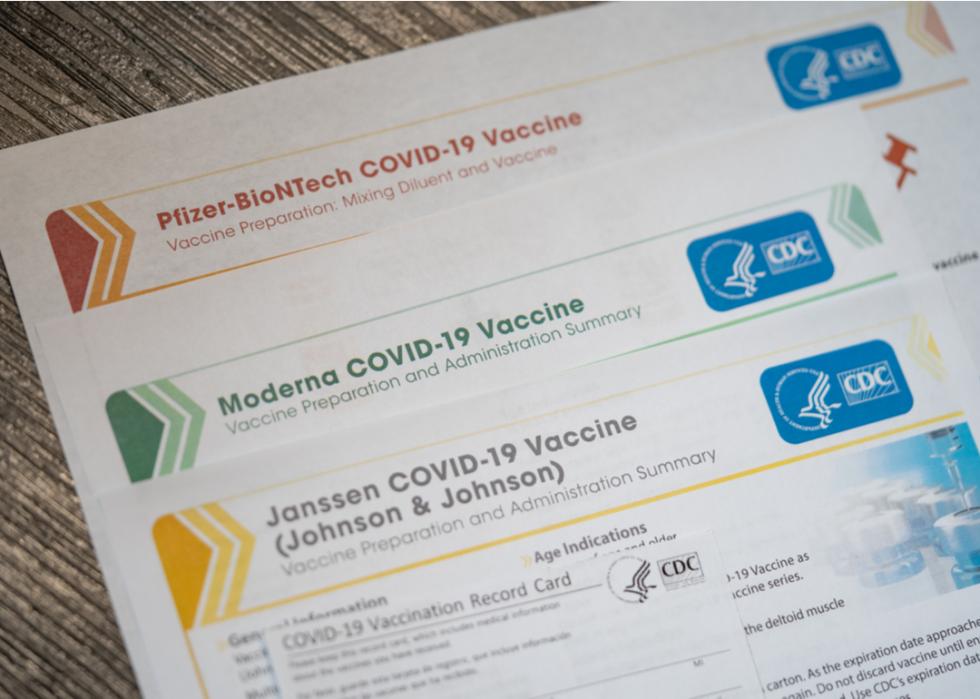
The Pfizer and Moderna vaccines are both mRNA (messenger RNA) vaccines that trigger an immune response. They use mRNA to instruct cells to make a harmless snippet of the spike protein that is found on the surface of the SARS-CoV-2 virus, which causes COVID-19. This protein triggers an immune response in the body, producing antibodies and protecting vaccinated people from getting infected if they are exposed to the real virus.
The Johnson & Johnson vaccine, instead of using mRNA, delivers instructions for cells with a disabled adenovirus that is not related to the coronavirus. The disabled adenovirus is unable to replicate in the body nor will it deliver a viral infection.
The Pfizer and Moderna vaccines each require two shots; the Johnson & Johnson vaccine is administered in a single injection.
COVID-19 vaccines are not interchangeable: If your first shot was from a Pfizer vaccine, the second one should also be Pfizer.

How do Pfizer and Moderna vaccines differ?
While the Pfizer and Moderna vaccines are both mRNA vaccines with similar efficacy (95% and 94.1% respectively), they have a few important differences. Key to these differences are the temperatures they’re stored at—Moderna at -4 degrees Fahrenheit, and Pfizer at -94 degrees Fahrenheit—and the time between doses.
The Johnson & Johnson vaccine can be kept at refrigerator temperatures for months at a time.

Are there any side effects?
All vaccines—similar to all medications—have side effects. Most COVID-19 vaccine side effects are mild, ranging from soreness at the injection site and headache to fatigue and fever. These side effects are completely normal and are a symptom of the immune response kicking in.
The Johnson & Johnson vaccine demonstrated an increased risk of a rare side effect involving blood clots with low platelets in women younger than 50. This risk was found to be far outweighed by potential benefits; after a brief pause of the vaccine in the early spring for further investigation, the vaccine was resumed April 23, 2021.
There have been very few serious allergic reactions to the Pfizer vaccine than to Moderna.

How did we develop vaccines so quickly?
These vaccines were able to be developed so quickly because the U.S. Congress directed nearly $10 billion to Operation Warp Speed, which was the project with the goal of producing and delivering 300 million safe and effective doses of vaccine by January 2021. That goal was not met by January. However, as of Sept. 9, 2021, 378 million doses of the COVID-19 vaccine had been administered in the U.S., according to data from Bloomberg.

How do we know these vaccines are safe?
These vaccines were approved in record time through emergency use authorization. However, they still went through all three phases of clinical trials in order to ensure safety and efficacy. In addition, the vaccine went through a manufacturing investigation and has been approved by the FDA. And as the vaccine is rolled out, it is monitored for any unexpected side effects.

What does 'emergency use' mean vs. full approval?
Emergency use authorization allows for the availability and employment of medical countermeasures such as vaccines during public health emergencies like the COVID-19 pandemic. Further FDA evaluations may lead to the full approval of such treatment, as in the case with the Pfizer vaccine.

Why are two doses necessary for some vaccines?
By giving multiple doses of a vaccine, the body has a chance to produce more antibodies against the virus because it is exposed to more antigens, which create more memory cells. This means that when the body is exposed to the real virus, it will have a faster and more effective antibody response. In the case of these two vaccines, administering two doses is the best way to create the most effective number of memory cells and antibodies.

How long does it take for the vaccine to work?
The Pfizer and Moderna vaccines offer immunity no less than 14 days after the final dose. It is so far unknown how long immunity will last, although experts consider efficacy to last for at least six months.

Should I get the vaccine if I'm pregnant or breastfeeding?
The vaccine was not tested on pregnant or breastfeeding people. However, the Food and Drug Administration in August confirmed the efficacy and safety of COVID-19 vaccines for those who are pregnant or breastfeeding.

Why have some people had allergic reactions?
In very few instances, the Pfizer vaccine has caused a severe allergic reaction. Scientists think this might be due to a compound, polyethylene glycol (PEG), used to package the mRNA. PEG has never been used in an approved vaccine, but it is found in drugs that occasionally trigger severe anaphylactic reactions. Some scientists are still skeptical of the causation.

Does the COVID-19 vaccine increase your risk for heart problems?
Up to 30% of patients hospitalized with COVID-19 present heart problems, according to the CDC. About one in every 6,000 teenagers receiving a COVID-19 vaccine have presented with rare heart inflammation cases; these cases have shown to be mild and resolve on their own. There is a much higher risk of heart issues from COVID-19 itself than from the vaccine.

Should I get the vaccine if I carry an EpiPen?
The CDC recommends that people with a history of severe allergic reactions should still get vaccinated, as long as their allergic reactions are not related to vaccines or injectable medicines. However, people allergic to polyethylene glycol (PEG) or polysorbate should not get the vaccine.

Are COVID-19 vaccines safe for kids?
The Pfizer COVID-19 vaccine is authorized for use in children between the ages of 12 and 15. Testing of the vaccines for safety and efficacy for children ages 2 and up is expected to yield authorization of COVID-19 vaccines for younger children in the coming months.

How far apart are the first and second doses?
In order to be as effective against COVID-19 as possible, both the Pfizer and Moderna vaccines require two doses. The Pfizer vaccine requires an interval of 21 days between doses, and the Moderna vaccine an interval of 28 days.
Johnson & Johnson’s vaccine requires just one shot.

Can COVID-19 vaccines cause cancer?
It is a myth that the mRNA vaccines change your DNA and can cause cancer. Because none of the COVID-19 vaccines interact with or change DNA, they are unable to cause cancer.

How are doses allocated to states?
According to an NPR article from November 2020, the government chose to allocate the first shipments of coronavirus vaccines based on population. This ignored a CDC proposal to distribute them based on high-risk groups. This is still how doses are allocated by state.

How does dose distribution work?
Distribution of the vaccine started 24 hours after the first emergency use authorization. Each week on Tuesdays, allocation lists are made available to states and jurisdictions so that they can order. Shipments then take place the following Monday. These orders won’t necessarily arrive all at once, but throughout the week. Sites get delivery notifications from private shipping partners.
Urban Indian Organizations and tribal health programs can elect to get vaccines distributed by the Indian Health Service or by the state.

How are vaccinations being counted?
Because the vaccine rollout is so localized, the numbers of vaccinations are tracked by a mix of interconnected state and federal databases. These data systems are utilized along with inventory management systems from FedEx and UPS, along with data management systems from Walgreens and CVS.
The CDC uses the cloud-based IZ Data Lake to manage incoming COVID-19 vaccine distribution and administration data from above-listed sources. All data are “deidentified” to protect the identities of those who have been vaccinated.

How many people have been vaccinated so far?
The up-to-date numbers on COVID-19 vaccinations can be found on the CDC COVID Data Tracker website. As of Sept. 15, 2021, a total of 179.3 million people were fully vaccinated.

Where can I get vaccinated?
Vaccines are administered through doctors, pharmacies, health centers, state and local health departments, and travel clinics. Because vaccinations are being handled locally and this information varies from place to place, visit vaccines.gov—the website from the Department of Health and Human Services—or your local health department's website for the most up-to-date information.

How much does it cost to get vaccinated?
Vaccine doses purchased by the federal government are available at no cost. However, vaccine providers may charge an administrative fee for giving the shot. This fee can be reimbursed by the patient’s insurance company.

Do I need to provide personal information?
While this answer varies somewhat by state and county, the CDC will collect personal information such as names, addresses, ethnicities, and birthdays of recipients of the COVID-19 vaccine. States have been asked to sign a data sharing agreement to hand over data taken at vaccination sites to the federal government.
Administration officials say that the data won’t be shared with other federal agencies; rather, it is needed to track effectiveness and adverse reactions should they arise.

Do we still need masks and social distancing after vaccination?
Even after receiving two doses of the COVID-19 vaccine, it will still be necessary to wear a mask and follow the other recommended hygiene and distancing protocols. This is because it will take time for everyone to be vaccinated and because, according to the CDC, “experts need to understand more about the protection that COVID-19 vaccines provide before deciding to change recommendations on steps everyone should take to slow the spread of the virus that causes COVID-19.”

Will schools require COVID-19 vaccinations for young students?
It’s highly likely. On Sept. 8, the Los Angeles Board of Education voted in favor of mandating vaccines for all students 12 and older who are attending in-person classes, making it the first major school district to do so. The rule, which will take effect in the second semester of this school year, requires all students to have had their first shots by Nov. 21.

Can my employer require me to get a COVID-19 vaccine?
Simply put, yes. Private companies have the right to institute mandated vaccinations for employees, as long as exemptions are allowed for medical or religious reasons. President Biden on Sept. 9 took things a step further by announcing a new, federal rule requiring all businesses with 100 or more employees to ensure all workers are vaccinated for COVID-19 or tested weekly for the virus.
More than half of all employers expect to roll out vaccine mandates by the fourth quarter of 2021, according to data from a survey released Sept. 1 by advisory and insurance firm Willis Towers Watson.



