
Depression is not an inherent part of aging: Here are 10 of the most common signs in older adults
Depression is not an inherent part of aging: Here are 10 of the most common signs in older adults
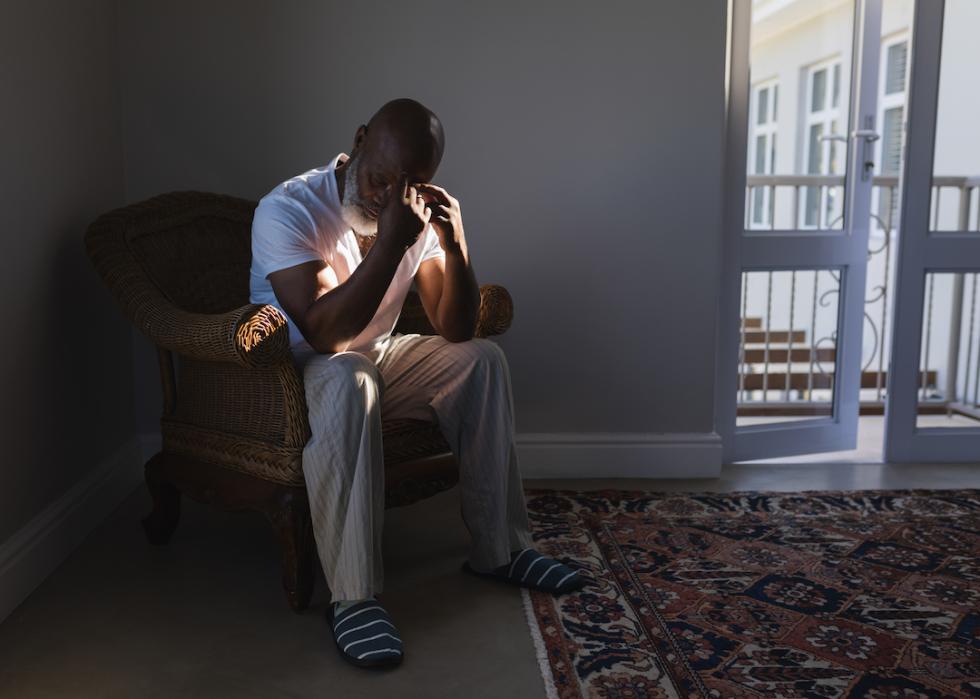
The American Psychiatric Association defines depression as "a common and serious medical illness that negatively affects how you feel, the way you think, and how you act," resulting in, among other symptoms, "feelings of sadness and/or a loss of interest in activities you once enjoyed."
Mental illnesses should be approached with the same seriousness and urgency as any physical disease. Unfortunately, depression in older adults is frequently misdiagnosed, undertreated, or mistaken as a natural sign of a person's "slowing down" with age or enduring chronic age-related physical ailments, of which an estimated 80% of older adults have at least one.
Stacker compiled a list of 10 of the most common signs of depression in older adults using information from the National Institute on Aging and other scientific and medical sources. Identifying these symptoms and seeking timely professional help can significantly improve the quality of life of older adults.
While depression rates among older adults are lower than among younger people, a lack of access to accurate information greatly increases the likelihood that older adults do not understand what is happening to them or how to ask for help. Depression in older people is often tied to cognitive changes, changes in sleep patterns, and a general loss of interest, all of which can contribute to a significantly higher risk of isolation. Family members, friends, caregivers, and health professionals in contact with seniors must therefore be aware of the warning signs in order to offer support and treatment options.
According to the Centers for Disease Control and Prevention, most older adults do not report feeling depressed, though living conditions and a person's degree of social interaction play a major role. While cases of depression among the elderly living within a community range from less than 1% to 5%, 11.5% of hospitalized patients and 13.5% of those who receive home health care have reported depressive symptoms.
Most elderly patients suffering from depression do respond to anti-depressive drugs, psychotherapy, or a combination thereof. Symptoms are usually different in seniors than in younger adults—they are less likely to develop cognitive-affective symptoms, such as dysphoria, worthlessness, or guilt than younger patients, while insomnia, fatigue, psychomotor lethargy, loss of interest in living, and hopelessness tend to be more prevalent.

Extended periods of feeling sad, anxious, or 'empty'
Grief and sadness due to the loss of a loved one or other life events are normal at all ages, but can become especially acute among seniors who outlive their siblings and friends. If the older adult is sad, anxious, or mentions feeling empty for a long period of time—more than a few months—they might be experiencing dysthymia or depression.

Consistent feelings of hopelessness, helplessness, worthlessness, or guilt
According to a study published by the National Library of Medicine, "self-worthlessness [or] inadequacy is a distinctive and consistent symptom of major depression across all cultures." The onset of these feelings is also a distinct reproducible predictor of a person's risk of recurrence after overcoming an initial bout of depression.

Restlessness or irritability
Seniors may show signs of being agitated, busy, or short-tempered by manifesting consistent nervous behaviors. They can repeatedly tap their fingers against a table, fidget, or repeat movements. They may also fixate on specific daily tasks such as cleaning and organizing, moving objects from one place to another, or making up excuses to try to leave the house. These and other demonstrations of restlessness, while a common symptom in Alzheimer's patients, can also be a sign of depression, especially when combined with episodes of irritability.

Loss of interest in hobbies and other pleasurable activities
Social withdrawal and a loss of interest in hobbies and other activities previously found pleasurable is called anhedonia, a core symptom of depression. Anhedonia can present as a social or physical symptom; social anhedonia is a progressive disinterest in interpersonal relationships and a lack of comfort in social situations, while physical anhedonia is the inability to feel tangible pleasures such as eating or touching.
Loss of energy or fatigue
Fatigue can make simple daily activities, such as getting out of bed or getting dressed, too hard to perform. It can be a consequence of suffering one or several other symptoms of depression, such as sleeping problems, indigestion due to bad food choices, or stress. It can also be a symptom on its own. One 2018 study found that more than 90% of patients with depression report feeling fatigued.

Sluggishness or moving and talking more slowly
While fatigue is the feeling of being exhausted even after sleeping or resting, sluggishness or lethargy can be a mental condition that compromises the capacity to move nimbly, even if the patient is physically able and healthy. It can affect speech, movement, and reflexes.

Memory and decision-making issues
In older adults, the loss of executive functions, memory, and the ability to make decisions can be symptoms of different diseases or just a normal part of the aging process. A health professional must accurately diagnose the patient to discard brain conditions such as dementia, infectious diseases, and chronic illnesses before attributing these symptoms to depression.

Sleep irregularity, including waking up too early or sleeping too late
According to the Sleep Foundation: "People with depression may find it difficult to fall asleep and stay asleep during the night or experience periods of excessive daytime sleepiness." The organization states that sleep problems and vice versa can exacerbate depression; sleep problems can bring on depression. Either way, there is an undeniable link between depression and sleeping. The sleeping habits of seniors must be closely supervised to prevent mental and physical health problems.

Change in appetite, especially with unintentional weight gain or loss
It is common for older adults to have less appetite since they have lower energy requirements due to less physical activity. There are several reasons for the elderly to lose their appetite: dental issues, difficulty chewing and swallowing, side effects of prescription medications, and depression. A mental health exam is recommended if a senior loses their appetite and weight for no apparent reason. On the other hand, if the person starts eating excessively, it might be a sign of stress or anxiety, conditions often linked to depression as well.

Suicide ideation or suicide attempts
A 2021 primer on the relationship between suicide ideation and suicide attempts pointed to, among other sources, a study by the World Health Organization that found "two‐thirds of individuals with suicidal ideation never make a suicide attempt." Mental conditions, such as depression, are strongly linked to suicidal ideation, but are not necessarily associated with suicide attempts. Constantly monitoring the elderly and providing them with adequate care and medical help is critical, especially if they have ever expressed suicidal thoughts.
Additional research by Emilia Ruzicka. Story editing by Brian Budzynski. Copy editing by Kristen Wegrzyn. Photo selection by Clarese Moller.



