In opioid crisis, race and stigma influence treatment
This story originally appeared on Ophelia and was produced and distributed in partnership with Stacker Studio.
In opioid crisis, race and stigma influence treatment
Despite more options to treat opioid use disorder, uneven access to effective treatments has furthered disparities in addiction and recovery along racial and economic lines.
For decades now, the United States has been ravaged by the opioid crisis, considered to be the worst drug epidemic in national history. Despite preliminary data showing a slight drop in opioid-related overdose deaths in 2023, the epidemic continues to wreak havoc on individuals and communities. According to data from the Centers for Disease Control and Prevention, nearly 80,000 people died from opioid-related overdoses between January 2023 and 2024, more than double the amount reported between January 2015 and 2016.
Ophelia analyzed data from the Substance Abuse and Mental Health Services Administration at the Department of Health and Human Services and other academic studies to examine disparities in access to opioid treatment in the United States and its ramifications for people in addiction recovery.
Deaths from opioid overdoses in the United States can be traced to three main waves. The first wave, following an increase in prescription opioids in the 1990s, triggered a rise in overdose deaths. By 2010, heroin-related overdoses surpassed those from prescription misuse, culminating in a new wave of overdose deaths. When illicit synthetic opioids like fentanyl entered the market in 2013, the third wave began, and it continues to plague the nation today. Overdose deaths involving synthetic opioids also spiked during the COVID-19 pandemic in multiple countries, according to the World Health Organization.
Further, opioid overdose deaths disproportionately impact Native Americans, Alaska Natives, and Black Americans. A 2022 Kaiser Family Foundation analysis of overdose death data shows Native communities are experiencing the highest death rates, which are increasing at much higher rates than those of any other ethnic group in the United States.

Racial differences in access to opioid treatment further disparities
Opioids refer to an entire class of drugs that are primarily used to reduce pain and can produce euphoric feelings. Included in this category are prescription pain relievers like oxycodone and hydrocodone, illegal drugs like heroin, and highly potent synthetic opioids like fentanyl and carfentanil. While these forms of opioids may differ in their intended uses and access requirements, they all have the potential for dangerous misuse that can result in addiction and death.
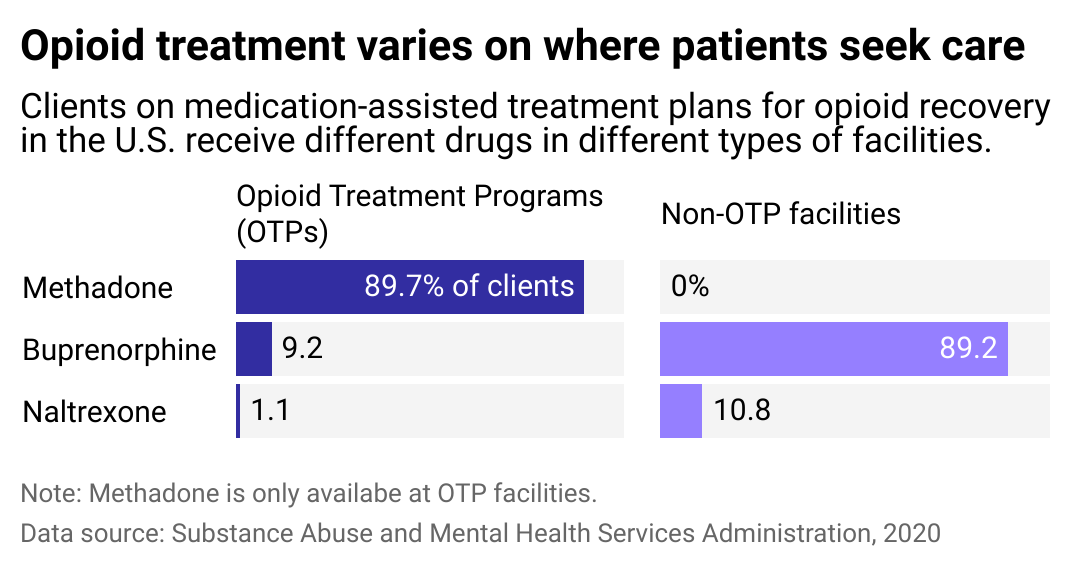
Race and income also impact the types of treatment that people suffering from opioid addiction receive. Both methadone and buprenorphine are drugs used to treat opioid addiction, but their usage and regulation are vastly different. Buprenorphine is classified by the Drug Enforcement Administration as a schedule III narcotic analgesic, which allows for at-home use. In contrast, methadone is classified as a schedule II controlled substance, meaning it has greater potential for abuse and, therefore, is highly regulated. Accordingly, methadone for opioid use disorder must be dispensed in daily dosage at methadone clinics or opioid treatment programs, which patients must frequent.
Methadone clinics have been shown to be predominantly located in low-income or Black or Hispanic/Latino neighborhoods and more readily accept Medicaid and Medicare. Buprenorphine providers, however, are commonly located in white neighborhoods. Access to the treatment also differs across economic lines and is largely utilized by patients with private insurance or the means to pay out-of-pocket.
Many of the stricter regulations toward methadone can be traced back to the war on drugs in the 1970s, a time when methadone clinics were seen as a crime-reduction tool. The punitive approach to addiction is still present in some of today's policies, addiction specialist Dr. Sarah Wakeman told Vox earlier this year.
"Even though now we're starting to talk about it [addiction] as a public health issue, our policies, our clinical approaches, our care models, our funding, really reflect this idea that we actually think people are doing something bad and so we should make it really hard on them," Wakeman said, who is medical director of the Mass General Hospital Substance Use Disorder Initiative.
In treating opioid addiction, today's public health experts and advocates emphasize a harm reduction approach, centering on the lived experiences of people who use drugs to prevent overdoses and associated health risks. Harm reduction incorporates various strategies to support well-being to address the opioid epidemic from all available angles.
These differences in legal classification and regulation between buprenorphine and methadone have led to material consequences for people seeking treatment for opioid use, which is why adopting a harm reduction approach is especially important after half a century of the "war on drugs" historical criminalization of people with addiction. These punitive policies led to mass incarceration for drug possession, which has disproportionately harmed Black, Hispanic/Latino, and Native people, who once arrested, receive harsher sentencing than their white counterparts. Although drug-related arrests among Black people decreased by 50% between 2009 and 2019, they are still two to three times higher than their share of the population, according to Pew Research.
Policies, programs, and approaches to addiction are all important components of harm reduction strategies in the opioid epidemic. One example is naloxone, an overdose reversal drug. Syringe access programs, which provide people with clean injection equipment to reduce the incidence of blood-borne disease and infection, are also extremely effective in achieving public health goals. Multiple cities have also implemented supervised injection facilities, where people can use substances under medical supervision, considerably reducing overdose fatalities.
Unfortunately, not all people have the same access to these programs and treatment opportunities, a consequence of racial discrimination that frames addiction in white communities as a medical disease and in nonwhite communities as a crime.
Regulation impacts how people can access care
While OTPs have historically only offered methadone, some facilities are beginning to provide buprenorphine to their clients. Over a third of clients at OTP facilities for veterans receive buprenorphine, as well as nearly a third of tribal government facilities. Even still, buprenorphine continues to be mostly accessible through non-OTP facilities, which becomes a barrier for the uninsured and unemployed.
Challenges in providing in-person health care during the COVID-19 pandemic led to changes in OTP treatment distribution. For the first time, telehealth, virtual screenings, and take-home dosages became available to access opioid use disorder treatment drugs. Initially designed to be temporary, these changes were made permanent by SAMHSA in April 2024.
More flexible options for accessing treatment could have profound benefits for patients who receive treatment drugs at OTP facilities, who frequently have to give up jobs and social obligations and incur expensive child care costs to maintain their required daily clinic visits. Full compliance with the updated OTP changes is expected to go into effect in October.
Story editing by Alizah Salario. Additional editing by Kelly Glass. Copy editing by Sofia Jarrin.