Roles in medicine projected to have the greatest shortages by 2035
This story originally appeared on QMedic and was produced and distributed in partnership with Stacker Studio.
Roles in medicine projected to have the greatest shortages by 2035
The COVID-19 pandemic revealed, among many things, the essential role medical workers play in our daily health and safety. One of the ways this manifested was in the recognition of a growing shortage of medical professionals.
In part, shortages have been—and will likely continue to be—driven by demographic change relative to demand. The U.S. population is expected to grow 10.6% by 2034, while the 65-and-over demographic will increase by more than 42%. This projected rise in the number of elderly residents will not only necessitate more sustained and specialized care for chronic conditions such as diabetes, dementia, and heart disease but more access to generalized care as well, given that those over age 65 seek physician care three to four times as much as younger people.
At the same time, a significant number of medical workers are leaving the profession either through retirement or as a result of the physical and mental toll the profession takes on them. Many workers who came out of retirement to work the front lines during the pandemic are once more retiring as the immediate threat recedes. The physical, mental, and emotional exhaustion can and has pushed qualified professionals to leave the field entirely.
One study published by the Mayo Clinic in September 2022 found that 63% of physicians reported signs of burnout, and the American Medical Association has characterized physician burnout as being at epidemic levels. Many medical professionals require up to a decade of education and training, and when burnout pushes fully trained professionals out of the field, it takes a long time to replace them.
Although shortages vary by region, some common threads tie this problem together. Difficulty in accessing care forces many Americans to seek emergency care as a last resort, putting a strain on emergency room workers and increasing patient costs. Shortages also may result in lower quality care, less face-to-face interaction with patients, longer wait times, and higher costs.
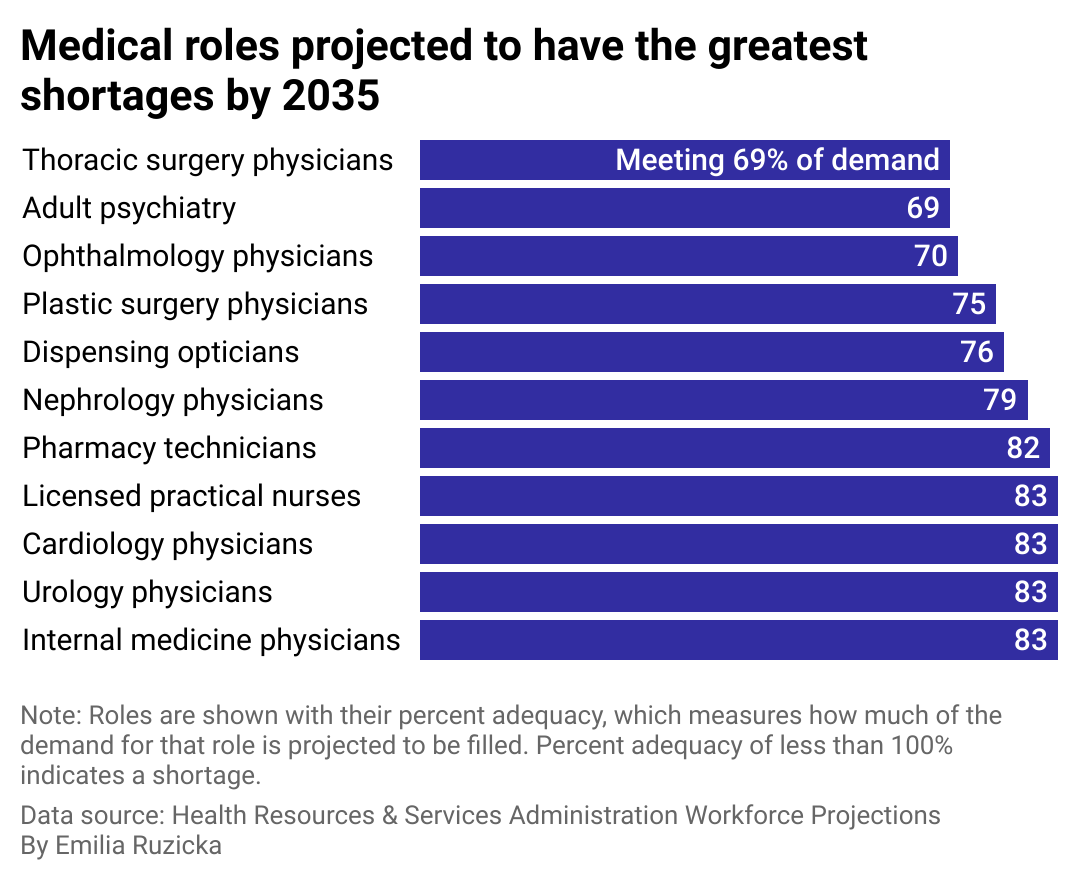
Using data from the Health Resources & Services Administration Workforce Projections, QMedic examined which roles in medicine are projected to have the greatest shortages by 2035.
Supply and demand in the medical field workforce
Medical specialties have unique supply and demand factors and face different obstacles in meeting demand. Overall, the specialties that can score Medicare-funded residency slots tend to produce more physicians and stand a better chance at meeting demand.
Nursing, which is projected to have among the highest shortages by 2025, is often plagued by many of the hardships and stressors that befall physicians but does not have as much funding support as other areas of medicine. Many nursing schools don't have enough faculty or access to clinical sites to accept the number of applicants they receive annually. Pay incentives are further driving this issue; most nurses qualified to teach can earn much more working in a hospital setting. Nurses have also reported growing rates of physical and verbal intimidation from patients.
The American Hospital Association recommends the federal government invest more money in nursing schools and salaries and put forth federal protections against violence in order to bolster the workforce and slow the stream of nurses leaving the profession.
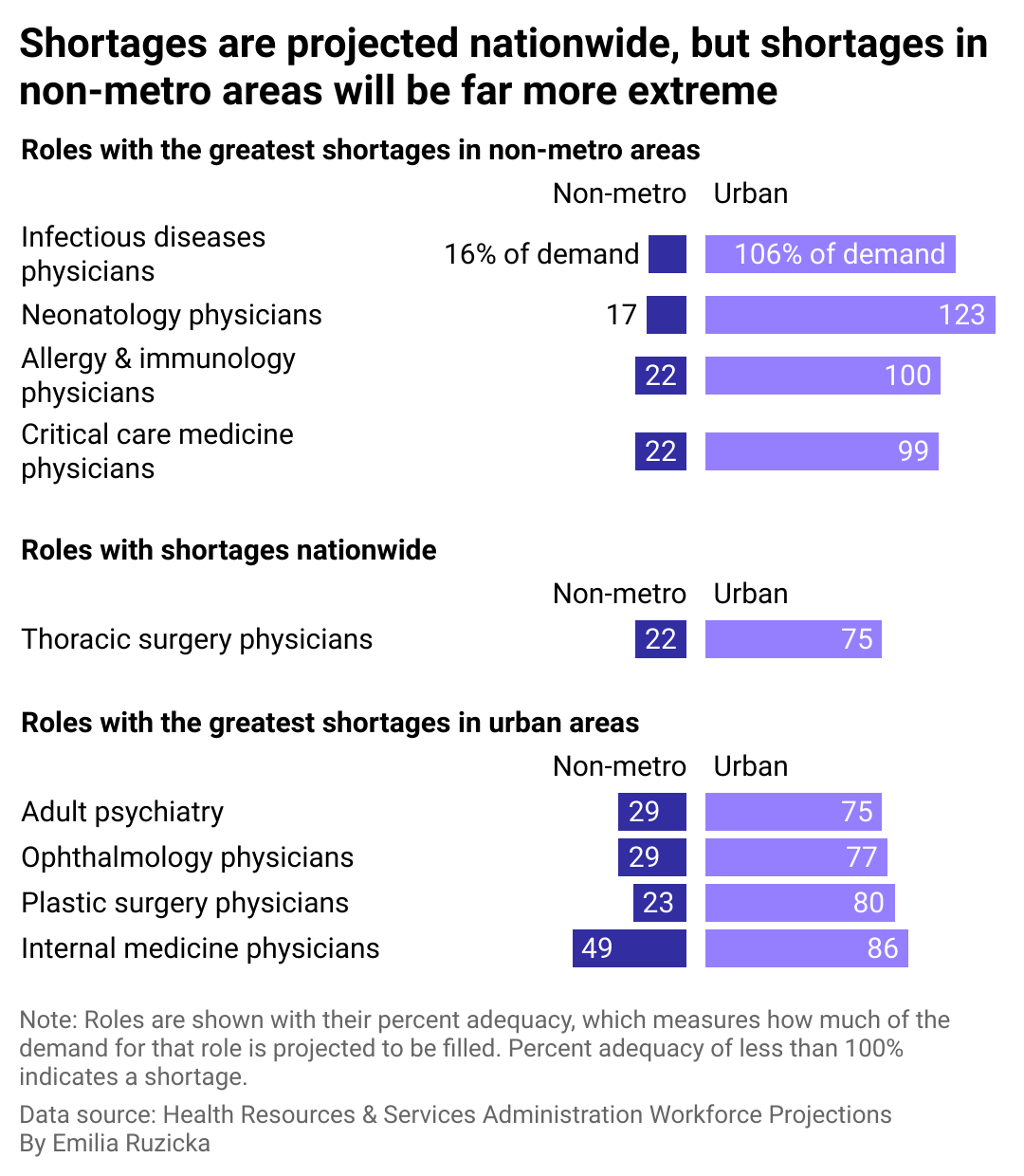
Effects of shortages heightened in rural America
Lack of proper health care and good hospitals exacerbates access issues that the roughly 46 million Americans who live in rural areas already face. Even before the pandemic, almost a quarter of rural Americans reported access to quality hospitals and doctors to be a challenge.
Additionally, people in rural communities tend to be older, less affluent, and underinsured relative to those in larger metro areas, and thus their heightened need for medical care collides with equally heightened financial challenges. Compounding the issue is the fact that rural medical facilities cannot generally afford to pay medical staff the salary they could expect in denser urban settings, which in turn has contributed to a dearth of available practitioners.
Most doctors practice at the location of their residency or within their resident facility's network, and most government-funded residencies are in urban medical centers. One result of this is so-called "doctor deserts" in many rural communities. The Association of American Medical Colleges reported in 2021, at the height of the pandemic, that three of every five federally designated health professional shortage areas were rural. As of July 2023, the Health Resources & Services Administration found that health professional shortage areas continue to be significantly more common in rural areas than urban ones.
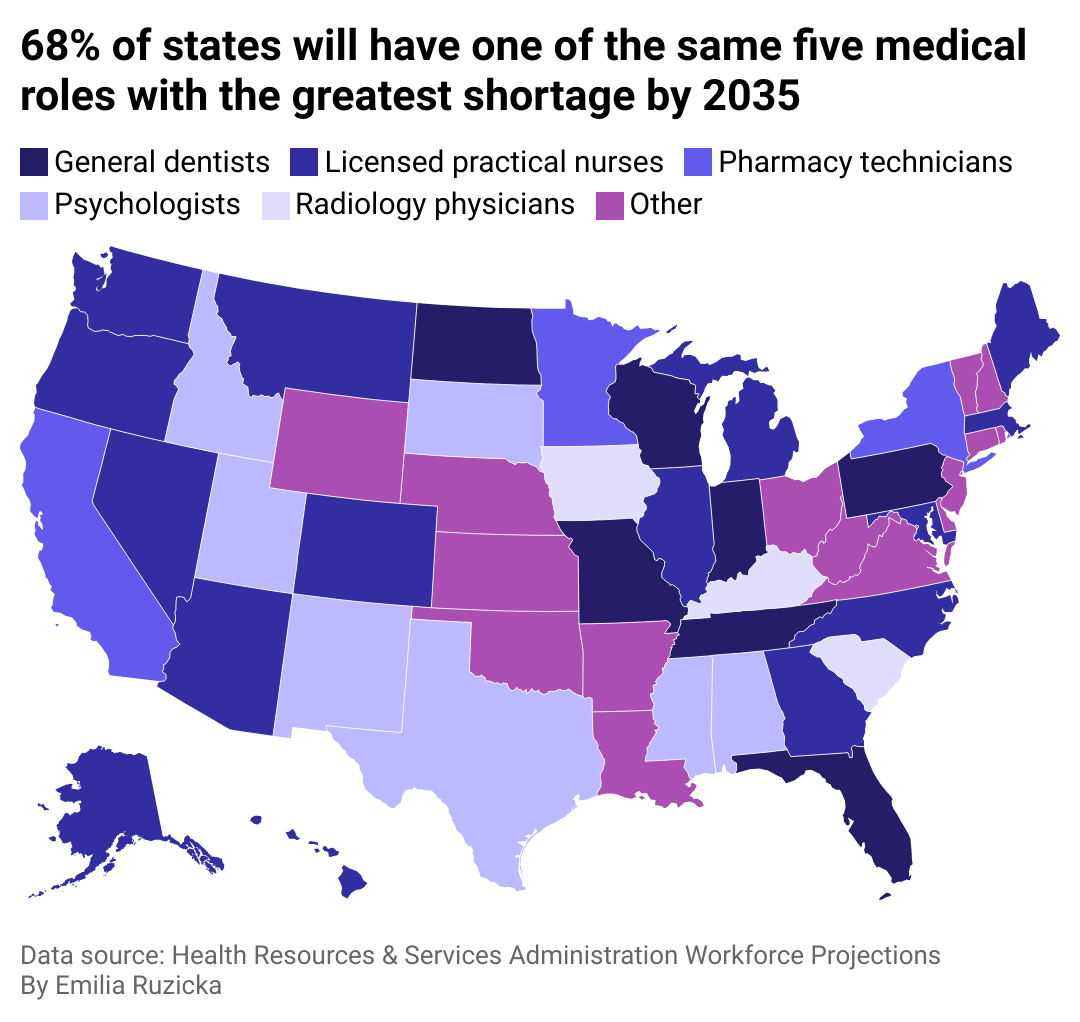
State-level trends and initiatives
Factors such as state population, geography, state-level policy, technology, and models of care all present varying landscapes for patients seeking care. Regionally, the South and West are projected to have the highest physician shortages. On a state level, California, Florida, and Texas are expected to experience the largest physician shortages, due in part to their anticipated population growth.
State-level solutions to address and reverse the shortages in medical roles across the U.S. largely focus on looser licensure and financial incentives. Cross-state licensing, which bloomed during the pandemic as a means of assisting physicians with telehealth work under the auspices of the Interstate Medical Licensure Compact, could mitigate shortages in some regions of the country. As of July 2023, 39 states and the District of Columbia are participating in the compact.
Some states have strategized to help relieve student loan debt in response to the shortages. Illinois, for example, repays up to $50,000 in student loans for nurses and physicians who agree to work in designated shortage areas in the state for up to four years.
Federal investment in the state shortages also plays a key role in addressing the shortages. In December 2020, Congress expanded support for Medicare-supported graduate medical education, appropriating funds to create 1,000 such positions over a five-year period in hospitals training residents over their cap or in states with new medical schools, teaching hospitals in rural areas, and hospitals that care for underserved communities. The following year, the Resident Physician Shortage Reduction Act was introduced, which would add 14,000 residency positions over seven years. The act was reintroduced in 2023 with bipartisan support and is pending Congressional approval.
Data reporting by Emilia Ruzicka. Story editing by Brian Budzynski. Copy editing by Tim Bruns. Photo selection by Clarese Moller.