Why does fentanyl exist? The history behind the substance driving record overdose deaths in the US
This story originally appeared on Ophelia and was produced and distributed in partnership with Stacker Studio.
Why does fentanyl exist? The history behind the substance driving record overdose deaths in the US
Fentanyl was the most promising medical advancement of its time. It's now one of the leading causes of death in the United States.
The highly addictive synthetic opioid has infiltrated illicit drug supplies and left holes in families across the nation. According to a New York Times analysis of Centers for Disease Control and Prevention data, fentanyl and drugs like it caused nearly 74,000 overdose deaths in 2022, surpassing other public health crises like car crash deaths and gun deaths.
It's spurred public policy initiatives in an attempt to stem the flow of fentanyl from China and Mexico. It's led to more regulation of prescription opioids and increased efforts to make opioid abuse treatments more widely available. It's also reigniting debates about how to prosecute drug crimes and how to compassionately treat those who have already become victims of its addictive grip.
Fentanyl is so frequently associated today with pain and suffering that it begs the question: Why was something so dangerous created in the first place? To get to the bottom of that question, Ophelia analyzed resources from academic journals, the Journal of Pain, and archived news articles to illustrate the origin of fentanyl, a drug that has become almost synonymous with America's opioid crisis.

A doctor's son and the father of more than 80 medicines
Paul Janssen was a revolutionary figure in Western medicine during the 20th century, developing dozens of medications and patenting more than 100 medical advances over his lifetime. The son of a doctor, Janssen lost his sister when she was only 4 years old after she contracted tuberculous meningitis.
During World War II, Janssen studied physics, biology, and chemistry in Belgium. His familial background and education in chemistry, in particular, inspired him to think about the potential for chemical sciences to be applied to advancements in medicine.
The time in which a young Janssen found inspiration was when war was driving innovation in health care at a rapid clip, and many procedures and medicines we take for granted today were just entering the fray. Surgeons were developing techniques to safely remove flesh so that fewer soldiers had to undergo amputation. Penicillin was seeing broader use for treating bacterial infections, having been discovered over a decade prior.
And Janssen, who would become known simply as Dr. Paul to colleagues, was plotting the creation of his independent research laboratory.

The quest for the 'most potent' narcotic pain reliever
The first open-heart surgery was performed in 1952, kicking off a period of surgical ambition that would inspire Janssen to formulate the chemical compound known today as fentanyl.
Around this time, doctors began experimenting with new techniques for heart surgery, the promise of treating heart disease propelling patients to take part in risky experimental procedures. Anesthetics available at the time often caused severe hypotension (low blood pressure) and arrhythmias (an irregular heartbeat) if they didn't kill the patient.
Janssen set out to formulate the "most potent" narcotic pain reliever ever made, synthesizing fentanyl for the first time in 1960. The drug was shown to have 100-300 times the potency of morphine, the primary drug used in surgical procedures at the time. Fentanyl also had fewer side effects for patients.
With morphine, the amnesia effect that helps patients forget the surgery while anesthetized was sometimes incomplete. Occasionally, morphine would also cause an allergic reaction; it also had the effect of depressing the respiratory system after surgery was complete, making it difficult for the patient to get oxygen. Fentanyl carries a similar impact on the respiratory system, and deaths from overdoses typically are the result of the respiratory system effectively shutting down.
Hurdles at the Food and Drug Administration
Fentanyl's potency worried some physicians, and that concern led to problems getting approval for its broader use. The Janssen Pharmaceuticals, acquired by Johnson & Johnson in 1961, struggled to get the Food and Drug Administration to approve the drug. It was resolved when Janssen suggested a 50:1 combination of droperidol and fentanyl be used in procedures, thereby diluting the chance for it to be misused because droperidol was known to induce a high that was not enjoyable.
The FDA ultimately approved the cocktail for use in the U.S. in 1968; four years later, fentanyl became available for use on its own in small quantities.

Fentanyl sales boom
Fentanyl's FDA approval paved the way for the drug's use in surgical settings in the 1970s, and its success in heart and vascular surgeries propelled it to widespread acceptance. The drug experienced a rare "blockbuster" moment in the 1980s, with medical sales growing 10 times in just its first year off patent in 1981. New drugs can be so expensive to research and develop that it's rarely profitable for a company to bring them to market unless they know sales will be immense.
Fentanyl had the added effect of activating pain-relieving and anesthetic responses in the body quicker than other methods of anesthesia. It was effective not only for surgical procedures but also for patients living with chronic pain and terminal illness. But all else aside, it was also easy and cheap to produce—and clinicians were leaning in.

Lollipops and patches hit the market
Its popularity in the medical community drove Janssen to develop other opioid anesthetics, which spurred companies to develop new ways of getting the drug into the patient's body throughout the 1980s and into the 2000s.
Companies introduced lozenges, lollipops, under-the-tongue sprays, and skin patches with varying use cases for patients depending on their pain relief needs. Some of these new technologies were commercial failures, but they broadened the use cases for the newly synthesized and extremely potent opioids.
The legacy of a medicine checkered with abuse
Since Janssen first conceived it in his lab, fentanyl has become the most widely used intravenous anesthetic for surgical procedures. At the same time, its excessive use began just years after the FDA first approved it in the 1970s. In the 1990s, overprescription of other opioid painkillers like OxyContin seeded the ground for the epidemic of opioid use disorder plaguing the U.S. today.
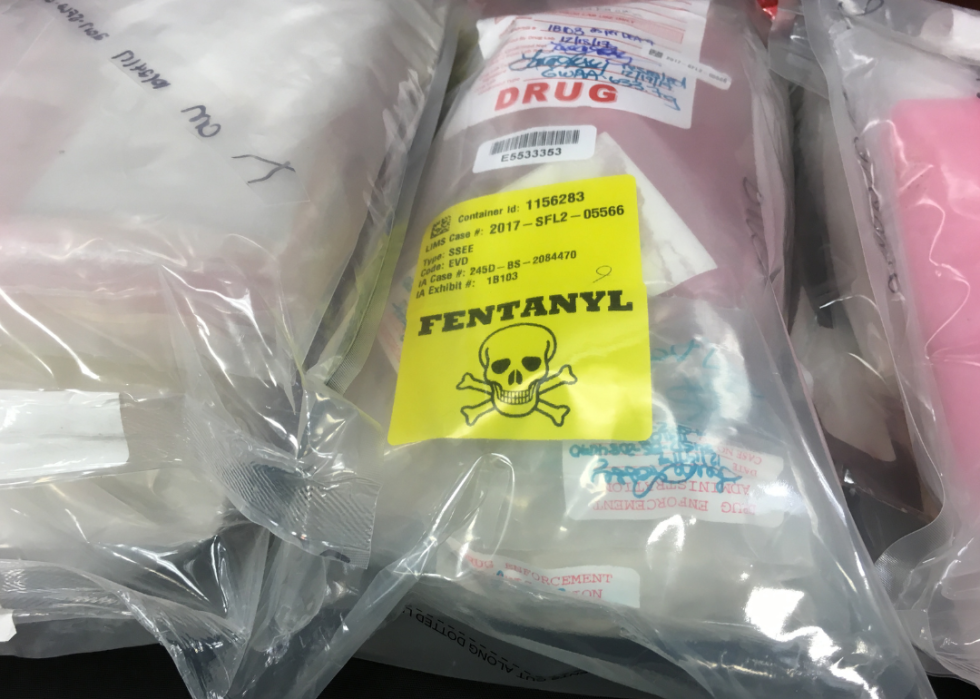
From the late 1990s through the 2000s, opioid-related overdose deaths skyrocketed, and regulators began cracking down on overprescribing physicians. Those efforts gave way to a rise in heroin overdose deaths in the early 2010s. And though fentanyl's potential for misuse concerned the FDA in the 1960s, it was perhaps impossible for regulators and the medical community to foresee the bevy of market forces that would lead to the modern-day opioid crisis in which fentanyl is featured heavily.
The drug's potency, synthetic origin, and ease of production—coupled with the advent of e-commerce in the 2010s—have made it so that black market actors could flood the market with illegally synthesized pills and powders. Today, any illicitly manufactured drug could be cut with fentanyl, and the prevalence poses a risk for those in recovery from opioid use disorder for whom one relapse could result in death.
Story editing by Ashleigh Graf. Copy editing by Paris Close.