
How compensation compares between Rhode Island staff and travel nurses
This story originally appeared on Vivian Health and was produced and distributed in partnership with Stacker Studio.
How compensation compares between Rhode Island staff and travel nurses
Heightened demand made nursing a high-paying profession over the last decade, especially since the COVID-19 pandemic began in 2020.
Nationally, registered nurses today earn more than $45 per hour on average—about $14 more than the average wage across all occupations in the United States. Traveling nurses with the same skills and credentials can earn another $16 more per hour, on average, compared to staff nurses. A typical contract for a traveling nurse is about 13 weeks but can be much shorter or longer.
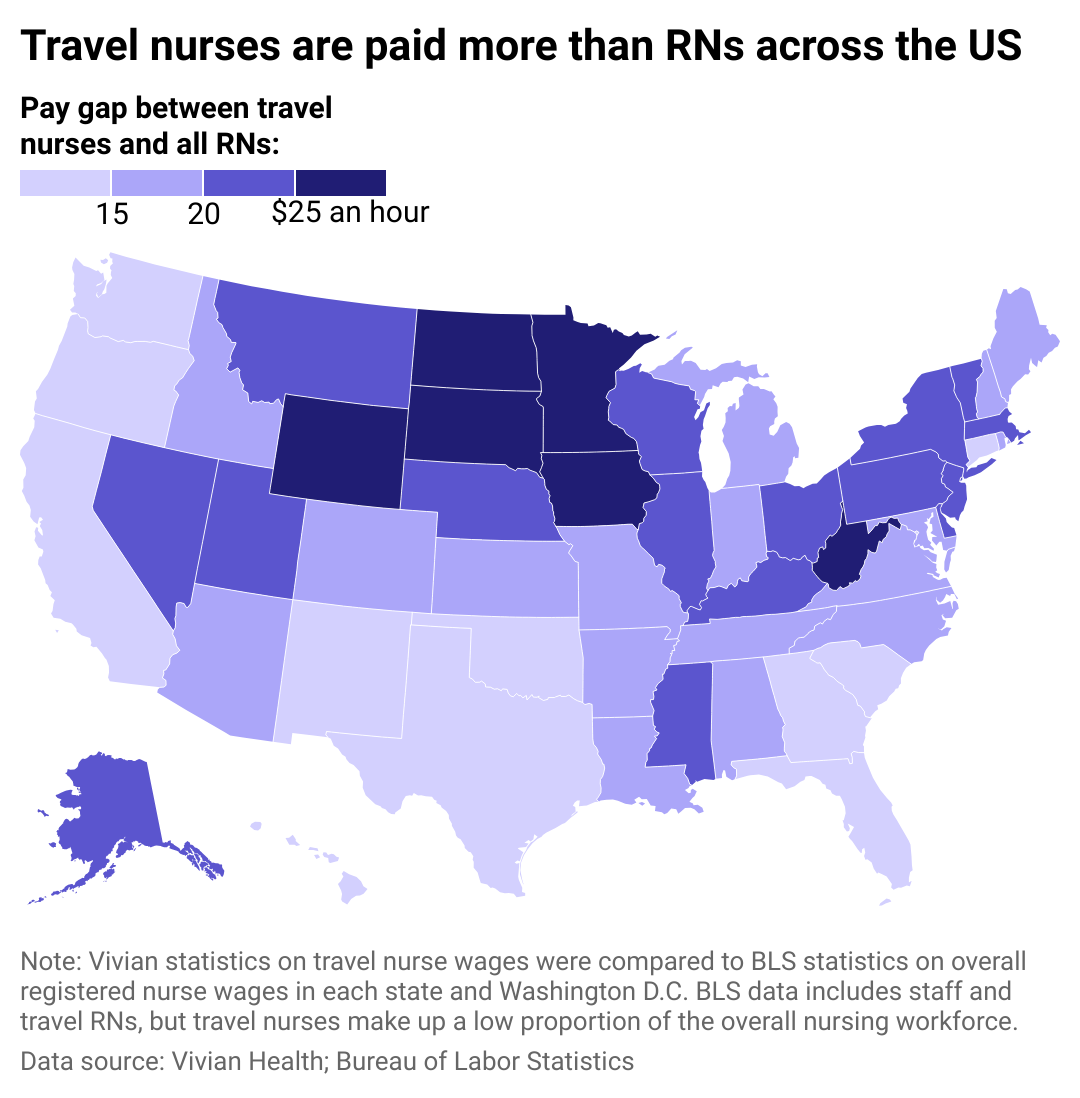
In some states, the pay discrepancy between travel and staff nurses is even more dramatic.
Vivian Health leveraged its own proprietary data, along with data from the Bureau of Labor Statistics, to analyze pay differences between staff and travel nurses in Rhode Island as part of a broader national analysis. Data from both sources was last updated in May 2023. BLS data on registered nurses is conflated with staff nursing positions in this analysis, though the numbers would technically include travel nurses, as well. However, travel nurses comprise a small portion of the overall RN workforce, and their wages won't affect the overall averages too much.
The pandemic exacerbated existing nursing shortages, driving high demand for RNs who could temporarily fill gaps. While COVID-19-related demand has eased, travel nurses remain a vital solution for ongoing nursing shortages.
How Rhode Island travel nurse compensation measures up
In Rhode Island, travel nurses earn $2,507 per week, or $62.68 per hour based on a 40-hour work week. That is $17.00 more per hour than registered nurses overall—on par with the difference in pay between travel nurses and all RNs nationally.
Across the nation, nurses who take travel contracts in the Midwest earn the most compared to their on-staff counterparts. Travel nurse pay stands out here, as a lower cost of living in this region often translates to lower compensation for residents. Offering high wages for traveling nurses in parts of the Midwest that are in need can help attract more RNs to these states, which are not ranked among the most popular for state-to-state migration. The Midwest enjoys higher ratios of nurses per capita than other areas in the U.S., which translates to less demand for travel nurses overall.
Conversely, the smallest differences in pay exist in the states where nurses are paid the most: Hawai'i and along the West Coast. These locations also have relatively high costs of living, particularly in urban areas, and strong nursing unions that help nurses demand better pay and benefits.
States on the West Coast are home to top nursing/medical schools and major medical employers, including Kaiser Permanente (California), University of Washington medical centers, University of California hospitals, and other large health care facilities. Nurses in California additionally benefit from legally mandated minimum staffing levels, which help prevent overworking and burnout.
Regardless of where they operate, travel nurses typically have the potential to earn much more than their staff counterparts. There are some downsides to these contracts, including a lack of stability, the challenge of learning a new workplace every few months, and less opportunity to build lasting relationships with co-workers and patients. But they also offer a chance to see new places, learn skills associated with various roles, meet many people, and build wealth.
Staffing up with temporary contracts, like those of travel nurses, created huge cost burdens for hospitals from 2020 through 2022. Many hospitals are in precarious financial situations to begin with and may need to rework their staffing strategies to be more sustainable. Still, amid nursing shortages and an aging, increasingly care-dependent population, travel nurses will likely continue to be a critical element of the American health care industry.
This story features data reporting and writing by Paxtyn Merten and is part of a series utilizing data automation across 51 states.



