How can you identify hidden behavioral health costs, and why does it matter?
How can you identify hidden behavioral health costs, and why does it matter?
You’re already paying for behavioral health. How much you’re paying might surprise you.
For many organizations, behavioral health costs don’t show up where you'd expect them. They’re buried in pharmacy spend, hidden in repeat disability claims, or camouflaged in high-cost ER visits. And because they aren’t always labeled clearly in your data, these costs go unnoticed—until they become unsustainable.
If you’re not connecting the dots between mental health needs and your rising medical spend, the real drivers of cost—and the most effective opportunities for savings—are obscured.
Spring Health brings them into focus in this story.
What are hidden behavioral health costs?
Hidden behavioral health costs are real, measurable expenses tied to untreated or unrecognized mental health and substance use issues. These costs show up across multiple areas of your business, but they rarely get categorized under “mental health.”
Instead, they’re hiding in places like:
- Pharmacy claims for antidepressants or ADHD medications, as well as higher indirect costs tied to treatment nonadherence, unmanaged side effects, or underlying chronic conditions.
- Emergency room visits triggered or exacerbated by mental health crises.
- Short-term disability resulting from depression, stress, trauma, or burnout.
- Neonatal and chronic care affected by poor mental health during pregnancy or while managing comorbidities.
In many cases, these costs are misattributed—treated as isolated medical issues rather than symptoms of unmet behavioral health needs.
How do behavioral health needs drive rising healthcare spend?
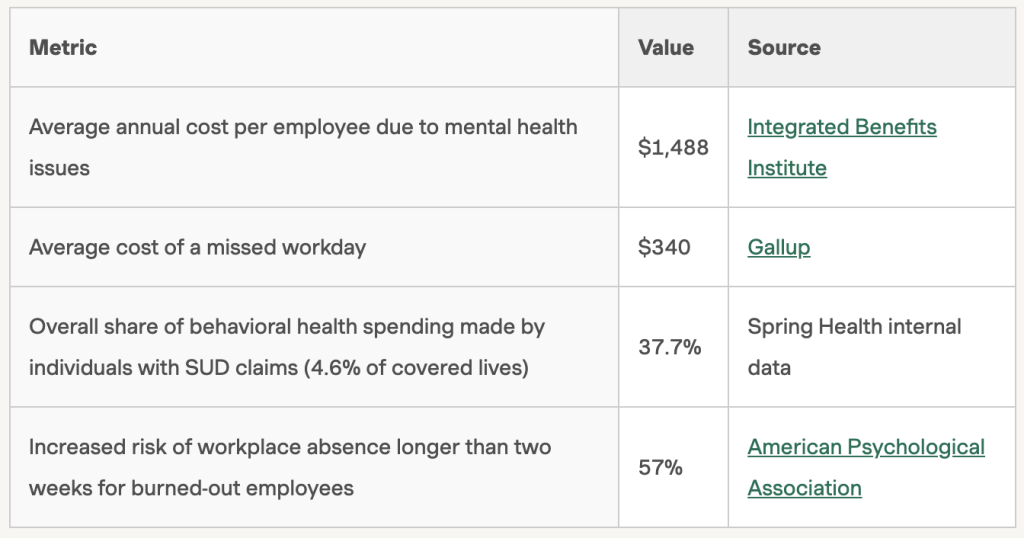
When behavioral health is left untreated or unsupported, it silently fuels higher medical claims, reduced productivity, and rising absenteeism and turnover. It’s a cost spiral that plays out behind the scenes in workforce data.
What does untreated behavioral health look like in the workplace?
Let’s make this real. Imagine three employees.
Marcus is dealing with insomnia and grief after a family loss. He takes multiple leaves of absence and goes on short-term disability, costing the company nearly $24,000.
Linda experiences anxiety tied to caregiving and financial pressures. She makes several ER visits and loses productivity—resulting in about $32,000 in costs each year.
Sarah struggles with performance issues and eventually leaves the company after a health crisis. Her departure and related costs total almost $100,000.
These aren’t extreme cases. They’re common patterns seen in workplaces across the country. And they’re often driven by unmet behavioral health needs.
How can you surface behavioral health trends in your claims data?
Here are questions to guide the conversation with your consultant or broker, along with the information that answers may reveal.
Can we isolate pharmacy claims related to behavioral health?
Helps identify medication spend related to depression, anxiety, ADHD, etc.
Are SUD costs broken out separately from general mental health claims?
Clarifies the true impact of substance use disorders.
How does our behavioral health trend compare to national or peer benchmarks?
Gauges whether your experience is typical or signals a problem.
What percent of high-cost claimants are receiving mental health care?
Assesses whether your sickest employees are getting support.
Can we overlay mental health data with chronic condition management?
Shows comorbidity impact on healthcare cost and outcomes.
Is our rising trend driven by demographics or addressable gaps in care?
Distinguishes between fixed versus solvable cost drivers.
What is our out-of-network behavioral health spend? Are there hidden costs in
under-spending categories?
Identifies opportunities to choose a solution where these costs are in-network. Costs could be hidden in medical claims, chiropractic, etc.
Many teams aren’t used to viewing their claims data through a behavioral lens. That’s okay. The key is to start asking the right questions—and push for clarity.
If you’re seeing rising costs and can’t explain them through traditional categories—don’t assume the data is lying. You might just be missing the behavioral thread that ties it all together.
Why are these costs so often overlooked?
In short: They’re mislabeled, fragmented, or deprioritized.
Most HR teams don’t have in-house resources for deep claims analysis. And when behavioral health is tucked under vague or inconsistent categories, even the best consultants can miss the pattern.
To make matters more challenging:
- Vendors may use different reporting bases (paid versus incurred claims).
- SUD and comorbidity costs may not be clearly tagged.
- Some partners may say their systems can’t support this level of insight.
But don’t settle for a surface-level view. Better data means better outcomes.
What happens when behavioral health is treated proactively?
Let’s return to Marcus, Linda, and Sarah. With targeted, timely mental health support, their stories change:
- Marcus gets trauma-informed care, improves sleep, and builds resilience.
- Linda works with a behavioral health coach who understands her caregiving challenges and finds new stability.
- Sarah receives specialized care, avoids hospitalization, and rebounds in her role.
And this isn’t just hypothetical. In real-world metrics and outcomes:
Return on investment (ROI): 1.9 times—for every $1 spent, employers save nearly $2 in health plan costs; amounting to $1,070 in net savings per participant in the first year.
Behavioral health utilization: +47% increase in employees accessing care—and getting it earlier in their care journey.
Total health plan savings: 30% gross reduction in combined medical spend (including hospital and ER visits); 14 % net cost reduction.
Cost reduction across chronic conditions: Highest savings observed in employees managing conditions like diabetes, chronic pain, and hypertension.
Why identifying hidden costs is a strategic imperative
Rising healthcare costs aren’t inevitable. They’re a signal—one that’s telling you it’s time to take a closer look at how behavioral health is showing up in your organization.
By proactively addressing mental health:
- You reduce avoidable claims.
- You retain your top talent.
- You build a more resilient, productive workforce.
Most importantly, you make an investment that pays off—not just in your bottom line, but in your people.
Bend the trend
Uncover the hidden behavioral health costs in your organization—and turn them into clear savings.
FAQ
How do behavioral health issues affect nonmedical costs, like productivity or retention?
The effects are significant. Mental health challenges can lead to absenteeism, presenteeism, reduced job performance, and turnover—costs that often exceed direct medical expenses. Employees struggling silently may disengage or leave entirely, creating ripple effects on team morale and business outcomes. Targeted behavioral health support helps retain high performers and keep teams functioning effectively.
What if our organization doesn’t have access to detailed claims data?
You’re not alone. Many midsized employers rely on brokers or consultants to interpret claims. Even without full access, you can still ask focused questions that surface behavioral health trends, such as:
- SUD breakout data
- High-cost claimant profiles
- Short-term disability patterns
Asking for a presentation on mental health trends is a great place to start.
How can we tell if our current behavioral health strategy is actually working?
Look for evidence beyond engagement metrics.
- Are your high-cost claimants getting the support they need?
- Has short-term disability decreased?
- Are ER visits and absenteeism down?
The most effective programs offer measurable outcomes—like ROI, symptom improvement, and cost savings tied directly to care engagement.
What’s the risk of doing nothing about hidden behavioral health costs?
Inaction comes with real consequences: unchecked medical spend, declining workforce wellbeing, and a growing gap between what employees need and what they receive. As stress, burnout, and mental health challenges rise across the workforce, addressing these needs isn’t just compassionate—it’s fiscally responsible. Choosing to act now positions your organization for a healthier, more sustainable future.
This story was produced by Spring Health and reviewed and distributed by Stacker.