How to reduce senior care overtime costs with optimized nurse scheduling
How to reduce senior care overtime costs with optimized nurse scheduling
For many senior healthcare organizations, overtime is viewed as a costly yet necessary part of day-to-day operations. Many different factors can affect workplace efficiency, staffing and patient demand in senior care, which only serve to potentially increase the amount of overtime needed.
Reducing overtime costs can be a crucial goal for healthcare organizations aiming to minimize unnecessary expenditure. However, with senior resident needs and quality of care to consider, nurse scheduling can quickly become a challenge that significantly affects patients, employees and organizations.
Understanding the reasons behind excessive overtime can help improve overall healthcare efficiency, leading to more informed business decisions related to senior patient care. To achieve this, many senior care companies are exploring advanced automated nurse scheduling solutions. But how can the information this technology provides be used to help save money, improve efficiency and reduce confusion in staffing and scheduling?
With so much to consider, understanding the causes, challenges and potential solutions to this issue can make all the difference. This guide by Smartlinx explores the main causes of overtime for nurses and how to reduce senior care overtime costs with optimized nurse scheduling.
What Are the Main Causes of Nurse Overtime?
Information and data can reveal opportunities to reduce expenditure. However, gaining more perspective on causation is equally important. Having a deeper insight into the main causes of nurse overtime is the first step toward reducing the associated costs.
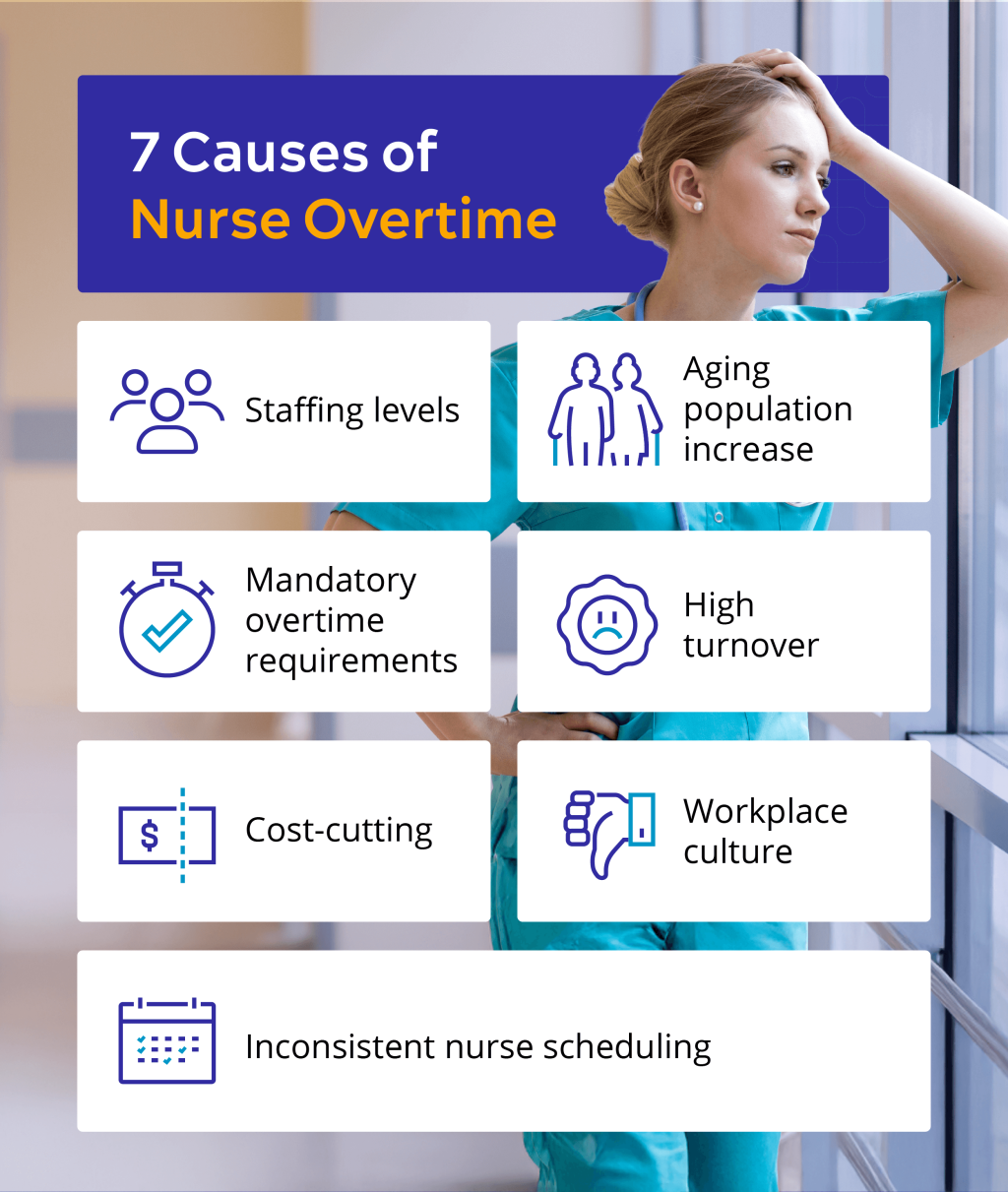
These factors can range from mandatory overtime expectations to institutional industry challenges that all senior healthcare organizations face. The following are some key causes of nurse overtime:
- Staffing levels: Inadequate staffing levels and increased patient demand can cause nurses to feel responsible for covering any gaps in care. This can mean having to stay late and pick up extra shifts to ensure elderly patients get the necessary help.
- Aging population increase: An aging population with increased care requirements means that nurses are spread thin and need to work overtime to meet these needs. This issue is likely to persist, as the number of Americans over the age of 65 is projected to reach 80 million by 2030.
- Mandatory overtime requirements: Some senior healthcare organizations implement mandatory overtime policies, which leaves many nurses with targeted overtime hours that they’re expected to meet as part of their role.
- High turnover: The high turnover rate of nurses due to burnout can create further staffing gaps, which in turn requires working nurses to cover these gaps. This can create a cycle of burnout, high employee turnover and the remaining nurses required to do more overtime.
- Cost-cutting: If a senior healthcare organization needs to reduce staffing or cut costs across the board, the remaining nurses may have to work more overtime than usual to keep the facility running as smoothly as possible.
- Workplace culture: Factors like a poor workplace environment and unsafe working conditions can all put pressure on nurses. This increased stress can lead to nurses changing careers and the remaining employees having to pick up the slack.
- Inconsistent nurse scheduling: Staffing levels that have been planned out in advance may not match patient needs, leading to nurses experiencing inconsistent or last-minute scheduling changes.
With a predicted 13 million nurses required to address the aging population and associated nursing shortages by 2030, these factors are expected to continue growing. For senior care organizations, this presents a unique challenge when exploring options to decrease overtime in healthcare.
How Does This Affect Senior Healthcare Organizations?
Reducing overtime in healthcare and the associated costs isn’t just something that directly affects nurses. These contributing factors can also have a negative impact on senior healthcare organizations through quality of care, reputational damage and lack of new applicants due to perceptions of a poor workplace culture.
Studies have also suggested that excessive overtime is one of the biggest contributing factors to higher rates of pressure ulcers in patients. Hospital-acquired infections like this may even be the basis for future medical malpractice lawsuits.
This cause-and-effect situation can potentially be resolved by understanding the things that affect nurse scheduling in senior care.
What Are the Common Challenges in Nurse Scheduling?
Scheduling shifts and staff cover accordingly is an important part of reducing overtime in healthcare and the associated costs. However, nurse scheduling can still present many challenges that need to be addressed before it can be effectively used to accomplish this.
Some common challenges that senior healthcare organizations face in nurse scheduling matters include:
- A lack of understanding in shift allocation: Many nurses aren’t given sufficient time between shifts for rest. When scheduling fails to account for consistently long shifts or frequent shifts between day and night, it can quickly cause fatigue or dissatisfaction among staff.
- Unexpected changes: Unanticipated events, like a sudden increase in senior patients or other nurses not showing up for their shifts, can make scheduling a challenge. They can also significantly affect planned schedules — nurses may have to change shifts or move to other units with little notice.
- Operational or staffing problems: Determining and predicting the patient-to-nurse ratio for seniors isn’t easy. It’s a balance that needs to consider skill levels and credentials, making it difficult to adjust to absenteeism or unexpected issues.
- Compliance: The Nurse Practice Act in each state sets licensing and competency standards that can influence nurse scheduling within senior care organizations. The Centers for Medicare & Medicaid Services (CMS) also enforces nurse-patient ratio requirements. When staffing or shift allocation problems occur, this can make scheduling the right team members even more difficult.
- Outdated technology: Manual nurse scheduling methods can lead to human errors, oversights and difficulties for nurses who want to check shifts or request changes. These systems can be outdated, slow and frustrating for organizations and nurses alike.
Nurse scheduling that’s integrated with modern technologies is a crucial part of delivering care.
What Are the Benefits of Using Nurse Scheduling Software to Reduce Overtime?
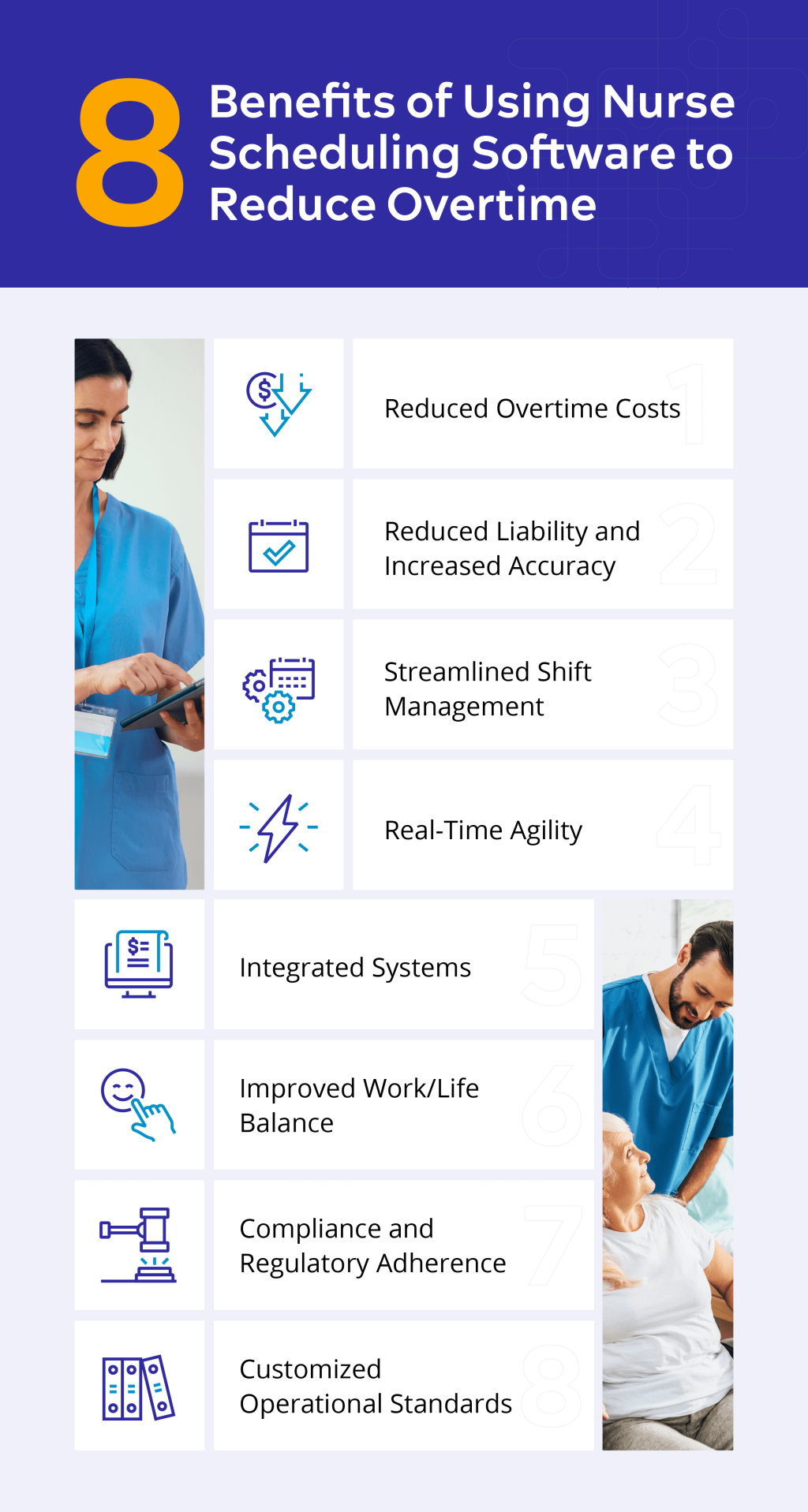
Understanding the long-term benefits of optimized nurse scheduling for healthcare organizations can help reduce scheduling issues. A study into the automation of nurse rosters for oncology care noted that the benefits of using nurse scheduling programming, which enhanced operational efficiency and the quality of care, could be applied to broader healthcare staffing solutions.
This presents an inviting opportunity for senior healthcare organizations seeking potential solutions to reduce overtime spending. Below are the benefits of using nurse scheduling software to address some of the common challenges.
Reduced Overtime Costs
The common challenges associated with nurse scheduling all contribute to additional overtime costs that healthcare organizations have to contend with. Making use of innovations like automated and predictive scheduling reduces the issues that come with having to schedule unexpected overtime.
The less overtime needed, the less overtime wages organizations will have to pay when it could’ve been avoided through nurse scheduling software.
Reduced Liability and Increased Accuracy
With so much information to process manually, outdated methods of nurse scheduling can leave considerable room for human error. Nurse scheduling software automates time-consuming tasks, such as shift scheduling, while also increasing accuracy by automating calculations.
In addition to reducing human liability, nurse scheduling software can also save a significant number of labor hours. This time saved can enable employees and senior healthcare organizations to allocate more hours to other key areas of care.
Streamlined Shift Management
Operational requirements in senior healthcare are always changing. In relation to these requirements, administrative tasks can quickly accumulate. Reducing overtime in healthcare can be a challenge when balancing daily work with constant rescheduling issues. Using nurse scheduling software can streamline administrative tasks and shift management, reducing confusion and creating a simple, cohesive system.
Every senior healthcare organization has its own specific requirements and demands. Embracing new technological solutions in long-term care can help alleviate administrative and staffing challenges by enabling quick rescheduling and updates.
Real-Time Agility
A lack of shift coverage and unexpected last-minute changes can significantly contribute to increased overtime costs. With optimized nurse scheduling software, data can be used to create fast and highly responsive adjustments to accommodate these needs.
Having agile solutions in place helps senior healthcare organizations remain responsive and flexible without compromising the overall quality of patient care. Nurses can also easily check their schedules for any changes, allowing them to better plan their week ahead and improve their quality of life outside of work.
Integrated Systems
It’s challenging to plan for long-term organizational cost efficiency with manual scheduling. Automated payroll and tracking management can help healthcare organizations stay ahead of potential overruns and maintain their financial targets by integrating systems to help monitor overtime management.
Integrated systems with in-depth overtime data to monitor cost efficiency and inform long-term financial planning helps maximize the value of a team while providing employees with more information and consistency. Nurses can also access pay stubs and request time off, while organizations can safely manage personal data and payroll information in one cohesive place.
Improved Work/Life Balance
Having access to innovative scheduling systems helps unify employees and organizations. It can ensure everyone is on the same page across the board. As it also makes sure that support, staffing and coordination needs are met, nurses can enjoy a clearly defined schedule to reduce worries, stress and frustration with unexpected changes.
This allows nurses to better plan their days off and feel less overwhelmed, while improving potential staff shortage risks to deliver the best possible senior care.
Compliance and Regulatory Adherence
Automated scheduling can help senior healthcare organizations avoid any CMS, state and government-mandated regulatory policy violations, while also ensuring that organizations stay on top of employee license expirations. Automated reports and time tracking can also simplify staffing and payroll compliance, helping busy organizations avoid unforeseen penalties.
This data can even be used to complete any potential CMS or governmental regulatory reports with just a few clicks and is easily exported to manual reporting destinations. The information the software captures on nurse attendance can also be cross-referenced with organizational attendance policies.
Customized Operational Standards
Healthcare organizations can use optimized nurse scheduling innovations to establish standardized rules tailored to their specific goals and needs. This can create features such as overtime capping or flags for early punch-ins and late punch-outs, all of which can be automatically set as time rules.
The ability to customize these new standards will help monitor performance, overtime hours and productivity.
Keeping Track of Reduced Overtime in Healthcare
You can decrease overtime in healthcare by understanding common challenges and leveraging the benefits of automated systems. However, keeping track of the overtime recorded and knowing which metrics to monitor is also important.
Having the right information to analyze helps senior healthcare organizations continue to identify trends, which can then be applied to cost-cutting plans. Some key metrics include:
- Total hours of overtime: Tracking the total hours of overtime worked over a given period (weekly, monthly or quarterly) offers a benchmark comparison to measure how much overtime increases or decreases within that set time frame.
- Overtime costs: Monitoring overtime costs can help identify and track any regular patterns where nurses are being asked to do overtime or request to do more overtime. This can help deliver long-term planning to reduce overtime costs and eliminate the patterns causing them.
- Overtime hours per employee: This tracking method ensures fair overtime distribution and helps identify trends or patterns that necessitate overtime. Once a pattern is identified, it becomes a key factor in reducing overtime.
- Employee productivity rates: Overtime hours may not accurately reflect the same level of productivity achieved during standard hours. Nurse fatigue can be a significant factor in determining this. Analyzing productivity by the hour can help highlight whether overtime hours are actually delivering efficiency in care.
- Task completion times: Tracking task completion times can help determine whether overtime has been actively increasing efficiency, and whether it is yielding a good return on investment. If it isn’t showing success, this insight helps healthcare organizations better understand the potential impact of reducing overtime on efficiency.
Reducing Overtime Costs and Increasing Efficiency in Senior Healthcare
Reducing unnecessary overtime and increasing efficiency are important for delivering quality senior medical care. Creating a more efficient, streamlined nurse scheduling system offers a wide range of potential benefits to senior healthcare organizations. However, it doesn’t stop there — it also extends to organizational costs. It can provide employees with clear information that they can regularly check to avoid staffing shortages and confusing last-minute changes.
By embracing modern scheduling technologies and knowing the long-term benefits of optimized nurse scheduling for healthcare organizations, senior healthcare leaders can pinpoint areas of improvement and identify the causes of unnecessary overtime. With a combination of understanding, clear processes and compliance needs all available in one platform, organizations can focus on delivering quality care from a motivated workforce.
This story was produced by SmartLinx and reviewed and distributed by Stacker.