
A crisis by the numbers: Nursing shortages in 2025 by state
This story was produced by Vivian Health and reviewed and distributed by Stacker.
A crisis by the numbers: Nursing shortages in 2025 by state
Global consulting firm McKinsey & Company predicted in 2022 that the United States would see a shortfall of 200,000 to 450,000 registered nurses, or RNs, for direct patient care by 2025. It appears the firm was correct. Between 2022 and 2025, the Department of Health and Human Services, or HHS, and Health Resources and Services Administration, or HRSA, noted a 1% increase in RN supply but a 3% increase in demand. The result was a deficit of about 295,800 nurses nationwide, falling within the predicted range. The persistent nursing shortage across U.S. health care systems is more than a temporary crisis. It's a consistent, critical challenge that strains hospitals and other healthcare facilities nationwide.
As the demand for healthcare services escalates with an aging population and ongoing health care reforms, the gap between the supply and demand of RNs widens, but only in some areas. Vivian Health compared data across all 50 states and the District of Columbia to perform a comprehensive analysis of where nursing shortages may continue to impact health care systems. This detailed examination explores the depth of the problem, pinpointing states facing the most significant shortages and those anticipated to have an oversupply for a quantitative view of the national distribution of nurses.
Nursing Shortages on a National Level
A study published in February 2024 by the JAMA Health Forum indicates the nursing workforce recovered in 2022 and 2023 following a substantial drop during the COVID-19 pandemic. It further emphasized that the workforce was on a trajectory to reach 4.56 million nurses in 2025, as previously forecast before the pandemic.
Other studies aren't in total agreement. While the most recent projections show nursing shortages easing, the gap between supply and demand decreases gradually over the 2027 to 2037 decade but doesn't fully dissipate.
The HHS and HRSA projected continued shortages of full-time equivalent, or FTE, RNs on a national level. They anticipate a 10% shortage in 2027, dropping to 8% by 2032 and 6% by 2037.
While the shortage wanes over the projection decade, a shortage still remains. The 6% shortage equates to about 207,980 FTE RNs nationally. Furthermore, the shortage spread is far from equal, with some states projected to have a surplus of nurses while others continue to face significant shortages.
Projected RN Shortages by State Through 2037
The HRSA generated its projections using historical data up to and including some 2022 data. Because the pandemic impacted the nursing workforce, this effect may only be partially captured in the data available for current projections. These projections assume that previous patterns of graduation, employee departures, and actively working nurses remain the same over the forecast period.
According to the HRSA's projections, the adequate supply of RNs significantly varies by state. The following 10 states have the largest projected shortages by 2037:
- North Carolina 22%
- Washington 22%
- Maryland 20%
- South Carolina 19%
- Michigan 19%
- New Mexico 19%
- Oklahoma 18%
- California 18%
- Idaho 17%
- Georgia 17%
Keep in mind that, like national projections, the projections for an entire state may still mean that certain areas are better covered than others. For example, the HRSA report released in November 2024 projects a 13% shortage in nonmetropolitan areas compared to just 5% in metro areas.
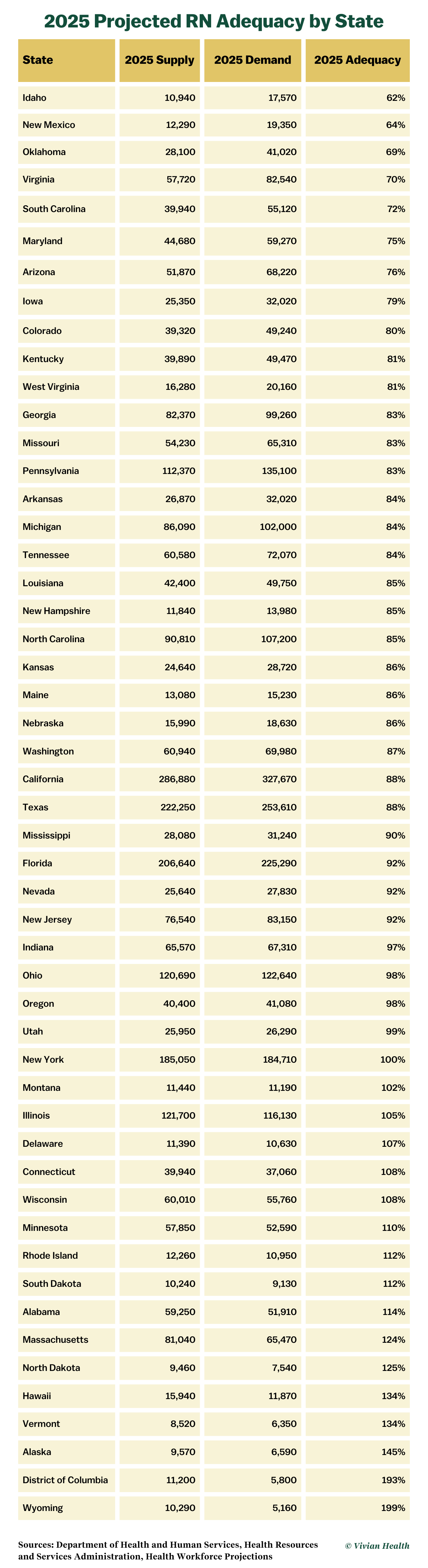
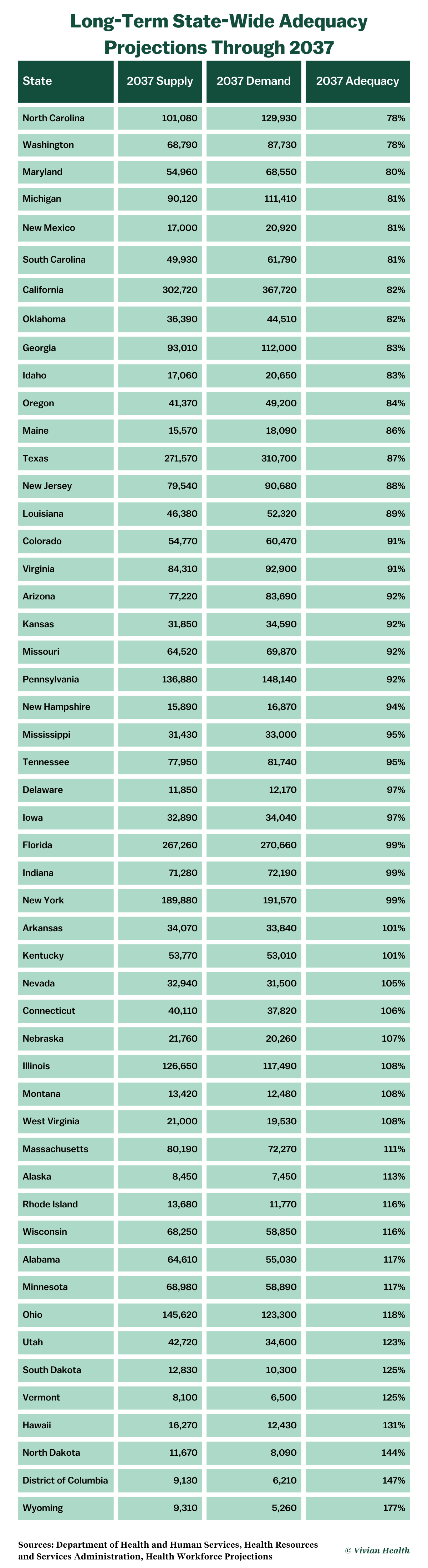
Vivian Health reviewed the HRSA's data to compare which states might see the gap in supply versus demand shrink between 2025 and 2037. It was found that 34 states would have a shortage in 2025 compared to 29 states in 2037. However, as some states' shortages improve, others worsen.
For example, North Carolina has an anticipated shortage of 15% in 2025, rising to 22% by 2037. Conversely, Idaho has an expected shortage of 38% in 2025, falling to 17% by 2037. On the opposite end of the spectrum, Wyoming is expected to have nearly double the nurses the state needs in 2025, with an oversupply of 99%, but it drops to 77% by 2037. To see how your state fares, see these two tables—one showing projected adequacy in 2025 and the other projected adequacy in 2037.
Of the 34 states with a shortage in 2025, all but nine see their supply increase in 2037. However, only seven of the 26 states with an increased supply end up with an oversupply, between 1% and 23%. Utah notably goes from 99% adequacy in 2025 to 123% in 2037, a jump of 24%. While this increase is less than West Virginia's jump of 27%, this state's overage is much lower at 108%.
On the flip side, six states see their adequacy drop even more—from 1% to 14%—between 2025 and 2037. Oregon has the largest projected decrease, dropping from 98% adequacy to 84% (still higher than North Carolina's 78%). Georgia and Maine are the only two states where adequacy doesn't change, remaining at 83% and 86%, respectively.
Fifteen states and the District of Columbia have overages in 2025, and the HRSA projects eight to see adequacy continue to rise, between 3% and 19%. North Dakota has the most significant climb, rising from 125% to 144%, the third-highest overage. Of the remaining eight that drop, six will still have an oversupply.
New York was the only state at an even 100% in 2025. It and Delaware are in the exception column, with New York dropping from 100% to 99% and Delaware from 107% to 97% in 2037, moving both states to the shortage category. No state was at an even 100% in 2037.
In 2037, HRSA projects that 29 states will still have a nursing shortage. However, three states—Florida, Indiana, and New York—will only be short by 1%. Of the 22 states with overages, Arkansas and Kentucky are only over by 1%.
Notably, the District of Columbia had the most significant decline in supply versus demand over the projection period but remained well above adequacy, decreasing from 193% to 147%. It continues to have the second-highest overage, with Wyoming's decrease of 22% keeping it firmly in the lead. Its continued surplus falls from 199% to 177%.
Nurses per Capita by State
To better understand how organizations determine whether a state will be understaffed or overstaffed, Vivian Health looked at nurses per capita, meaning the number of nurses for every 1,000 persons in a state's population, and used 2023 data from the Department of Labor, or USDOL, and the Census Bureau (the most recent available from the USDOL) to calculate RN per capita for each state and ranked them from lowest to highest.
The national per capita was 9.43 RNs for every 1,000 residents. Using this figure, you could assume that any state with less than 9.43 RNs per capita would be considered as having a nurse shortage. Using this premise, 23 states were below the national rate. However, since there's a national RN deficit, the per capita nationwide is technically also too low.
This table provides the RN per capita in each state and the District of Columbia.
Licensed Versus Actively Working
Another aspect to consider is that there are likely many more licensed RNs than there are actively employed and those employed may not be employed at the bedside, potentially impacting shortage data. Furthermore, RNs may hold multiple single-state licenses but can only work in one place at a time. These nurses may be counted as part of the workforce in several states, potentially skewing the numbers further to some degree. Travel nursing jobs can also muddy the waters, especially if an RN has a multistate license through the Enhanced Nurse Licensure Compact from her home state but frequently works in other states instead.
Vivian explored the differences between active RN licenses posted by the National Council of State Boards of Nursing versus employed RNs from the USDOL in 2023. You can compare those differences in this table.
What About Other Types of Nurses
While the bulk of our investigation covered RNs, Vivian Health also looked at the projections for licensed practical/vocational nurses, or LPN/LVNs, and nurse practitioners, or NPs, to understand the outlook for these nursing professionals. The HRSA projects the demand for LPN/LVNs to grow faster than supply, but the opposite for NPs.
In its nurse workforce report, nationwide projections for LPN/LVNs would result in a shortage of 302,440 FTE LPNs by 2037. The HRSA indicated the projected supply of LPN/LVNs would only meet 80% of demand in 2027, and this adequacy would fall to 72% by 2032 and 64% by 2037. Like RNs, LPN adequacy varies greatly by state, ranging from an astounding 80% shortage in Maine to a 17% overage in West Virginia by 2037.
Supply was anticipated to exceed demand for NPs, resulting in a 26% overage by 2027, rising to 53% by 2032 and 76% by 2037. However, distribution among states remains a factor. For example, California opened a pathway for NPs to practice without physician supervision to help alleviate the state's ongoing primary care clinician shortage. California projects a shortage of 8,000 primary care clinicians by 2030, which includes doctors, physician assistants and NPs.
What's Causing Nursing Shortages?
In the wake of the COVID-19 pandemic, the number of nurses with the intent to leave their jobs was high but expected to wane. However, it stayed higher than many expected. Many health systems have seen the anticipated turnover occur, with an overall decrease in the active nursing workforce.
While several of these systems have had some success in rebuilding their nursing workforces, others haven't. Estimates in early 2023 still suggested a shortage of nurses nationwide, especially within acute-care settings.
The continuing nursing shortage is a multifaceted crisis with deeply rooted systemic challenges and current issues with equally significant impacts. At its core, the nation's aging population demands more healthcare services while the nursing workforce ages in parallel, leading to a monumental retirement wave.
Concurrently, a persistent bottleneck in nursing education hindered by faculty shortages limits the number of new nurses entering the profession. Based on data from McKinsey & Company, experts don't expect the educational pipeline to be able to keep up with demand. This shortcoming is expected to result in a gap between nurse graduates and job openings of more than 800,000 in 2031.
Specific factors contributing to the complexity of the nurse staffing deficits include:
- Aging population: The baby boomer generation, one of the largest generational cohorts, continues to age. By 2030, all baby boomers will be 65 or older, and as this population segment ages, the demand for complex care and nurses to provide this care increases.
- Aging workforce: Like those they serve, the nursing workforce is also aging, with an estimated one million RNs retiring from the workforce between 2017 and 2030. The impending retirement of a large chunk of nurses threatens to sharply reduce the experienced nursing workforce in less than a decade.
- Increased burnout: Nurses are experiencing burnout at unprecedented levels due to high-stress environments, long hours, and continued staffing shortages. The intense pressure has led to decreased job satisfaction, increased absenteeism, and many nurses leaving or considering leaving the profession altogether.
- Nurses leaving bedside jobs: An increasing number of nurses are leaving high-stress bedside positions for alternative roles in health care or different industries altogether. Commonly cited reasons for nurses leaving the bedside include burnout, unsafe staffing ratios, inadequate support staff, being underpaid and underappreciated, the inability to take breaks or adequate days off, and insufficient mental health resources. In February 2023, the National Library of Medicine reported that the average nursing turnover rate nationwide was 8.8% to 37%, depending on the specialty and geographic location.
- Faculty shortage: According to the American Association of Colleges of Nursing, nursing schools turned away nearly 92,000 qualified applicants for baccalaureate or graduate nursing programs in 2021. This number was the highest in decades and primarily due to capacity issues, including insufficient clinical sites, classroom space, faculty, and clinical preceptors. Unfortunately, the salaries for faculty roles aren't very competitive, making them less attractive to qualified instructors.
- Economic incentives in other fields: Competitive wages and less stressful working conditions in other sectors lure away trained nurses who might otherwise remain in nursing careers or attract potential nursing professionals from the field, reducing the number of entrants into nursing programs.
- Violence in the healthcare setting: The presence of emotional or physical abuse in healthcare settings further adds to an already stressful environment. Violence in nursing has become an ever-present threat, from psychological trauma to varying degrees of bodily injury, including death. Healthcare workers are five times more likely to sustain an injury due to workplace violence than other professions.
How Nurse Demand and Shortages Impact You
Nursing shortages confronting health systems are well documented, but the data isn't always in agreement on the severity of the issue. Discrepancies between findings can be attributed to variations in data collection methods, changes over time not consistently reflected among studies or reports, and differences in local or regional impacts. Furthermore, projections assume that historical patterns of graduation, labor force participation, and departure from the labor force remain unchanged over the entire forecast period.
Bear in mind that many factors can impact supply and demand, so a projected surplus can quickly become a shortage and vice versa. Many issues can influence whether parameters stay the same for a decade, which is why annual updates are necessary and why Vivian Health updates this post each year as new data becomes available.
No matter what the data indicates, there will always be a constant need for healthcare services and RNs and other nursing professionals to provide these services. Whether you're a travel nurse or a staff nurse looking for a change of scenery, knowing which states expect to have a surplus of nurses versus those facing shortages can help narrow your options.
States with nursing shortages will likely pursue recruitment strategies beneficial to nurses, such as offering higher salaries, better benefits, flexible scheduling, and other incentives to attract nurses to the area. On the flip side, states with a surplus of nurses may not offer the most competitive wages or the perks you want.
Some healthcare employment locations have historically paid more than others with or without a shortage. However, higher costs of living often offset these inflated salaries. When comparing your relocation options or travel assignment locations, make sure the salary is a livable wage.



