
5 big changes to Medicare coming in 2026
5 big changes to Medicare coming in 2026
Medicare enrollees can expect new rules and benefits in 2026. Even if you have original Medicare, which tends to have stability in hospital and medical coverage, you should be aware of changes to premiums, deductibles, and other out-of-pocket costs. If you have Medicare Advantage, which is a private alternative to original Medicare, you should expect even more updates to your coverage. It’s also important to track changes to your prescription medication benefits known as Part D.
The Medicare & You 2026 handbook can give you a broad overview of the program.
GoodRx shares more about big changes for the 2026 coverage year.
Key takeaways:
- Medicare Part D changes in 2026 include a higher out-of-pocket maximum, lower prices for the 10 medications subject to Medicare Drug Price Negotiation, and auto-renewal for people who were enrolled in the Medicare Prescription Payment Plan in 2025.
- Original Medicare enrollees in six states will be subject to prior authorization for certain Part B items and services during a six-year pilot program that begins in 2026.
- You will have a special option to change Medicare Advantage plans if you used the Medicare Plan Finder to choose coverage, but note by early 2026 that the directory information in the online tool contained errors — and you find that your preferred doctors and hospitals aren’t covered by your plan.
What’s changing with Medicare in 2026?
If you have Medicare, here are five updates in 2026 that will likely affect you.
1. Medicare Part D out-of-pocket limit increases to $2,100
Part D is Medicare coverage for prescriptions, devices, and some vaccines. As recently as 2024, the out-of-pocket maximum was $8,000. A new plan design removed the “donut hole” — a pause in prescription coverage — and limited an enrollee’s annual out-of-pocket expenses to $2,000 in 2025. That cap increases to $2,100 in 2026. After you spend that much, your Part D plan pays 100% for covered medications for the rest of the year.
2. Part B prior authorization pilot starts in 6 states
Prior authorization is common for prescription plans. But this advance approval process was rarely used for medical services covered by original Medicare. Advance approvals are far more common for people who have Medicare Advantage plans.
But beginning in January 2026, a six-year pilot program of coverage reviews will begin for some original Medicare enrollees. Prior authorization will be required for certain Medicare Part B services and items received in six states: Arizona, New Jersey, Ohio, Oklahoma, Texas, and Washington. The Part B services and items subject to these coverage denials have been deemed potentially wasteful and prone to fraud by the federal government. The pilot program doesn’t apply to Medicare Part D plans, which already use prior authorization and step therapy.
3. Automatic renewal for Medicare Prescription Payment Plan enrollees
The Medicare Prescription Payment Plan, which debuted in 2025, gives anyone with Medicare prescription coverage the option to make payments for out-of-pocket costs instead of spending up front at the pharmacy. This program continues in 2026, and participation remains voluntary. What’s new in 2026 applies to people who signed up in 2025. You will be automatically renewed for participation unless you opt out.
4. A chance to change plans for inaccurate Medicare Advantage directory information
The Medicare Plan Finder can help you compare Medicare Advantage plans and Part D plans. The 2026 coverage year is the first time this online tool has included a provider directory for each plan. This information is helpful for people who have preferred healthcare professionals and medical facilities. The provider directory for each plan should be accurate, but it may include healthcare professionals and facilities no longer in network. That means you could use flawed information to make a decision. If this happens to you after using Medicare Plan Finder information with directory errors, you can be eligible for a special election period to choose a different Medicare Advantage plan. You must catch the issue within three months of the coverage beginning (typically by March 31) and call 1-800-633-4227 (1-800-MEDICARE). With confirmation that you received incorrect information with the Medicare Plan Finder, you have these options:
- Choose a new Medicare Advantage plan (with or without Part D prescription coverage).
- Disenroll from Medicare Advantage and return to original Medicare.
- Choose a Part D plan, which will automatically return your medical coverage to original Medicare.
Coverage will start the month after you make a new plan selection.
5. Medicare drug price negotiation lowers costs for 10 medications
The Medicare Drug Price Negotiation Program, activated in 2023, was one result of the
Inflation Reduction Act of 2022. For the first time, Medicare could work with drug manufacturers to reduce the prices of high-cost prescription medications. The first round of negotiations included 10 brand-name drugs covered by Medicare Part D that treat conditions such as diabetes, heart failure, and psoriasis.
Lower prices for the following medications were effective on Jan. 1, 2026.
Negotiated Medicare prices for 10 drugs in 2026
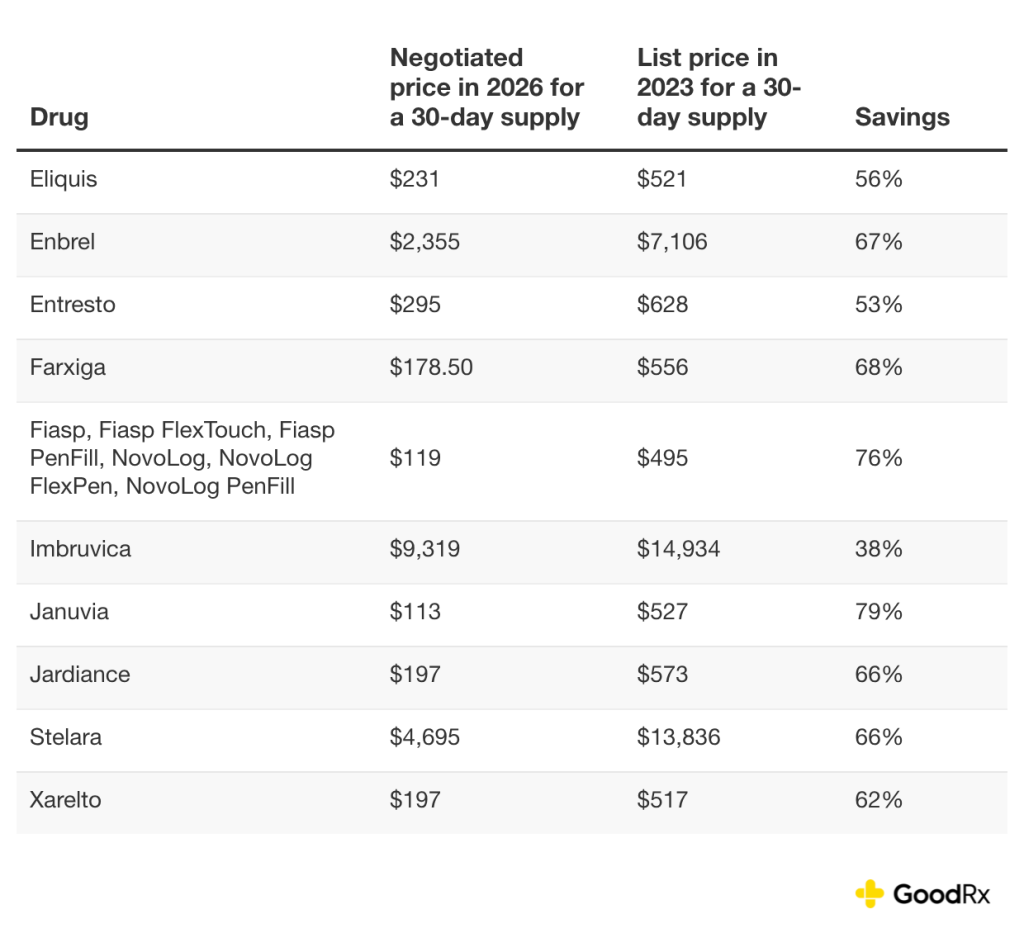
These 10 medications must be on the formularies of all Part D plans.
Anyone with Part D coverage could save on out-of-pocket costs if they take any of these 10 medications. You should expect to pay less if your cost-sharing is coinsurance, which is a percentage of the price. Enrollees with fixed copays could also pay less.
There are negotiations underway to lower costs for an additional 15 medications in 2027. Medications covered by Part B medical insurance will be included in the list effective in 2028.
Will you pay less for Medicare out-of-pocket costs in 2026?
Probably not. Standard premiums, deductibles, and other Medicare out-of-pocket costs are increasing for the 2026 coverage year. Your Part D premium may be lower if you stay in the same prescription plan you had in 2025. If you take a medication included in the Medicare Drug Price Negotiation program, your costs may decrease.
How are prior authorization rules changing?
As part of a six-year pilot program that begins in 2026, you may face prior authorization for certain Part B services and items if you live in:
- Arizona
- New Jersey
- Ohio
- Oklahoma
- Texas
- Washington
Prior authorization will not apply to inpatient or emergency services and won’t be used for care that would pose a substantial health risk if delayed. The services and items that may be subject to prior authorization include:
- Arthroscopic lavage and arthroscopic debridement for the osteoarthritic knee
- Cervical fusion
- Deep brain stimulation for essential tremor and Parkinson’s disease
- Diagnosis and treatment of impotence
- Electrical nerve stimulators
- Epidural steroid injections for pain management, excluding facet joint injections
- Hypoglossal nerve stimulation for obstructive sleep apnea
- Incontinence control devices
- Induced lesions of nerve tracts
- Percutaneous image-guided lumbar decompression for spinal stenosis
- Percutaneous vertebral augmentation for vertebral compression fracture
- Phrenic nerve stimulator
- Sacral nerve stimulation for urinary incontinence
- Skin and tissue substitutes, such as bioengineered skin substitutes, for lower-extremity chronic nonhealing wounds and wound application of cellular- and tissue-based products for the lower extremities
- Vagus nerve stimulation
Are there any Medicare plans discontinuing in 2026
Most Medicare enrollees will have slightly fewer Medicare Advantage options in 2026. Medicare enrollees will be able to choose from an average of 32 standard Medicare Advantage plans with Part D coverage and seven standard Medicare Advantage plans without Part D for the 2026 coverage year. (These figures exclude special needs plans and other specialty coverage options.) That means there are fewer options, on average, than the 34 standard Medicare Advantage plans with Part D and eight standard Medicare plans without Part D that were available to an enrollee in 2025.
Some states are alerting consumers about the possibility that their plans may be dropped for 2026.
The bottom line
Expect changes in 2026 if you have original Medicare or Medicare Advantage medical and hospital benefits — and especially if you have Medicare Part D prescription medication coverage. Medicare Part D will have a $2,100 out-of-pocket maximum in 2026 (which is $100 higher than 2025), but lower prices for the 10 medications subject to Medicare Drug Price Negotiation. People who joined the Medicare Prescription Payment Plan in 2025 will be auto-renewed in 2026.
A six-year pilot program will test prior authorization for original Medicare enrollees in six states for certain Part B items and services beginning in 2026. And you’ll have a special election period in 2026 if you used the Medicare Plan Finder to select a Medicare Advantage plan but found out the online tool contained directory errors and your preferred healthcare professionals and facilities aren’t in network for the plan you chose.
This story was produced by GoodRx and reviewed and distributed by Stacker.



