How the One Big Beautiful Bill affects your healthcare
How the One Big Beautiful Bill affects your healthcare
On July 4, 2025, President Donald Trump signed into law the budget reconciliation package known as the One Big Beautiful Bill Act (OBBBA). This law makes some of the most significant changes to the U.S. healthcare system in years, and it affects Medicaid, Medicare, Affordable Care Act (ACA) coverage, and employer-sponsored benefits.
Some people may face new rules to keep their health insurance. Others may gain more flexibility through tax-advantaged accounts. Understanding what’s changing — and when — can help you avoid coverage gaps and unexpected healthcare costs, GoodRx, a platform for medication savings, reports.
Key takeaways:
- The One Big Beautiful Bill Act makes major changes to Medicaid. These include new work requirements, tighter eligibility checks, and new cost-sharing copays.
- New verification rules will require some Affordable Care Act (ACA) marketplace enrollees to reverify eligibility. Also, repayment caps for excess subsidies will be removed, and the law did not extend enhanced ACA subsidies, which are scheduled to expire after 2025.
- Several other healthcare changes are also on the horizon. These include more ACA marketplace plans becoming HSA eligible and updates to Medicare drug price negotiation rules.
- Most changes go into effect from 2026 to 2028.
How does the Big Beautiful Bill affect health insurance?
The OBBBA makes major changes to how people get and keep health insurance, especially through Medicaid and ACA marketplace coverage.
Medicaid is a joint federal-state program that provides free or low-cost health coverage to more than 70 million low-income adults, children, older adults, and people with disabilities. ACA marketplace coverage refers to private health insurance plans purchased through HealthCare.gov or state exchanges. This often includes income-based premium tax credits.
Health policy researchers and federal budget analysts expect that the law’s insurance-related provisions could lead to millions of people losing coverage over the next decade. The biggest impacts are expected to come from new Medicaid work requirements, stricter eligibility and verification rules, and the expiration of enhanced ACA subsidies.
Estimates from the Congressional Budget Office and other health policy researchers suggest the following impacts:
- Medicaid work requirements. More than 5 million people could lose health insurance by 2034 as a result of new work and reporting requirements.
- More frequent eligibility checks. About 700,000 people could lose Medicaid coverage because some enrollees will have to prove eligibility every six months instead of once a year.
- Expiration of enhanced ACA subsidies. Around 22 million people, including 5 million small-business owners and self-employed workers, could see higher marketplace premiums in 2026 if enhanced subsidies expire as scheduled.
- Loss of marketplace coverage. About 4.2 million people could become uninsured by 2034 if ACA coverage becomes unaffordable.
Many of the health insurance changes in the OBBBA are scheduled to go into effect from 2026 to 2028.
What are the major One Big Beautiful Bill healthcare changes?
Not every provision in the law affects consumers in the same way. Some changes directly affect coverage eligibility and out-of-pocket costs. Others change how specific programs and benefits operate. Below are the most significant, consumer-facing healthcare changes in the law.
1. Medicaid work requirements
Many adults aged 19 to 64 enrolled in the Medicaid expansion program will be required to complete at least 80 hours of work or community engagement activities per month to keep their coverage. States will have to verify compliance at least twice per year. People who do not meet the requirements could lose Medicaid even if they still qualify based on income.
The law includes mandatory exemptions, such as for people who are medically frail, disabled veterans, pregnant individuals, and certain caregivers. But people who qualify for an exemption may still need to submit paperwork or documentation to confirm their status.
States that expanded Medicaid under the ACA will be required to implement these rules by January 1, 2027. But states may adopt them earlier. Georgia is the only state with a Medicaid work requirement in effect. It launched its program in 2023 under a federal waiver.
2. Medicaid cost-sharing copays up to $35 per visit
Adults in the Medicaid expansion population may face copays of up to $35 per visit for certain services. This is the first time that Medicaid enrollees may have regular cost sharing for covered care. But total cost sharing is capped at 5% of household income, which limits how much enrollees can pay overall.
Some services remain exempt, including primary care, prescription medications, rural health clinic services, and several other categories.
3. Stricter verification rules for ACA marketplace subsidies
People who receive ACA premium tax credits will need to complete pre-enrollment verification before coverage starts. This includes confirming income and eligibility in advance, rather than after enrollment.
These rules may limit automatic reenrollment for some marketplace enrollees, meaning people may need to reverify eligibility or reapply each year to keep their subsidies.
4. No cap on excess ACA subsidy repayment:
Premium tax credits are subsidies that help lower the monthly cost of ACA marketplace health insurance for people with moderate incomes. These credits can be paid in advance to lower monthly premiums (called advance premium tax credits) or claimed later on a tax return.
Under the new law, there is no longer a limit on how much excess advance premium tax credit a marketplace enrollee may have to repay if their income ends up higher than expected. Previously, repayment caps applied to households earning under 400% of the federal poverty level. Starting in 2026, those caps will be removed.
5. Medicare eligibility restrictions for certain individuals
The law changes who can newly enroll in Medicare by narrowing eligibility for some noncitizens who previously qualified. Under the new rules, Medicare enrollment is limited to specific immigration categories. Some people who would have qualified in the past will no longer be eligible to enroll.
Additional Medicare-related changes, including delays to enrollment assistance programs and updates to drug price negotiation rules, are discussed in more detail below.
6. Enhancements to tax-advantaged accounts
Starting in 2026, the dependent care flexible spending account (FSA) contribution limit will increase from $5,000 to $7,500 per household. A dependent care FSA is an employer-sponsored benefit that lets workers use pretax dollars to pay for eligible child care or dependent care expenses, such as daycare or after-school care. The higher limit applies only if an employer updates its plan design to allow the increased contribution.
The law also expands access to health savings accounts (HSAs). HSAs are tax-advantaged savings accounts that allow people with qualifying high-deductible health plans (HDHPs) to set aside money for medical expenses. Contributions are made with pretax dollars, grow tax-free, and can be withdrawn tax-free when used for eligible healthcare costs.
Under the new law, bronze and catastrophic ACA marketplace plans will qualify as HSA-eligible plans. This change allows more people to use HSAs to save for medical expenses with tax advantages.
Are there Medicare cuts in the Big Beautiful Bill?
The broad healthcare cuts in Medicaid and the ACA will affect many Medicare beneficiaries indirectly, including those who are eligible for both Medicare and Medicaid. Here are some provisions that may reduce or limit certain types of Medicare support:
1. Delaying improvements to Medicare Savings Program
The Medicare Savings Program (MSP) can help people who have lower incomes pay Medicare costs, such as premiums, deductibles, and coinsurance. A 2023 Centers for Medicare & Medicaid Services rule would have streamlined MSP enrollment and eligibility processes, reduced administrative burdens, and made it easier for people to keep their coverage. But the OBBBA delayed implementation of this rule until 2034.
2. New rules for Medicare eligibility requirements
OBBBA changes who is allowed to enroll in Medicare. Before this law, many lawfully present immigrants could qualify for Medicare if they worked and paid payroll taxes long enough or if they met certain eligibility rules. Now, only certain groups can sign up for Medicare, including:
- U.S. citizens
- Lawful permanent residents (green card holders)
- Cuban and Haitian entrants
- People from certain Pacific Island nations with special agreements with the U.S.
People who can no longer enroll in Medicare include:
- Refugees and people granted asylum
- People with Temporary Protected Status
- Survivors of human trafficking
- Survivors of domestic violence
- Individuals granted humanitarian parole
By July 2026, the Social Security Administration must identify people who already have Medicare but do not meet the new immigration rules. These individuals will be notified that their Medicare coverage will end in January 2027.
3. Limits on Medicare drug price negotiation
In 2022, the Inflation Reduction Act (IRA) gave Medicare the power to negotiate prices for some high-cost prescription medications. But the law made an exception for orphan drugs, which are medicines used to treat rare conditions that typically affect less than 200,000 people in the United States. These medications were exempt from price negotiations only if they were approved to treat one rare condition.
But if a company studied its orphan drug for a second rare condition, the drug could become eligible for negotiation. Because of that, some manufacturers slowed or paused research into new uses. A report from the National Pharmaceutical Council found the number of orphan drugs approved for multiple conditions was cut in half after the IRA took effect.
The new law broadens the orphan drug exemption. It allows orphan medications with one or more rare-condition indications to remain exempt from Medicare price negotiations. These changes apply to Medicare drug prices beginning on January 1, 2028.
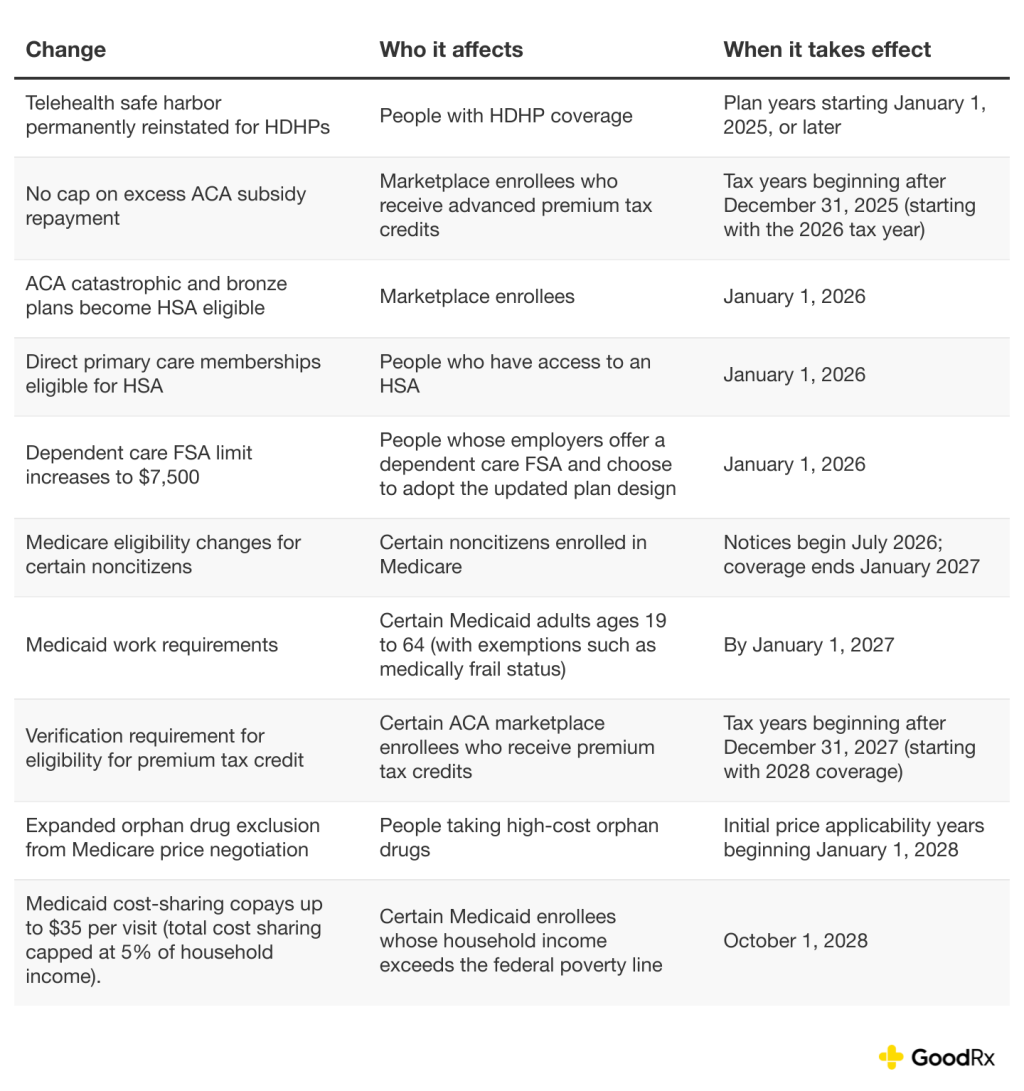
When do the Big Beautiful Bill healthcare changes go into effect?
The timeline below highlights when major healthcare changes discussed in this article take effect, along with a few health-related provisions in the OBBBA:
The bottom line
The One Big Beautiful Bill brings many changes to healthcare, including Medicaid, Medicare, and the Affordable Care Act marketplace. Some people may see higher premiums and new requirements to maintain enrollment while others may find more flexibility with their tax-advantaged health accounts, such as health savings accounts and dependent care flexible spending accounts.
Understanding when these changes take effect can help you prepare for open enrollment and avoid unexpected healthcare costs.
This story was produced by GoodRx and reviewed and distributed by Stacker.