
As more parents abstain from vaccinations, children from low-income households may pay the price
This story originally appeared on Northwell Health and was produced and distributed in partnership with Stacker Studio.
As more parents abstain from vaccinations, children from low-income households may pay the price
For many American children, it's a rite of passage: Visit the pediatrician for a routine checkup, get a quick jab in the thigh or upper arm, and go home with a brightly colored bandage, a lollipop, and lifelong protection against a dangerous and deadly disease. Vaccines, one of the most important public health advances of the 21st century, have nearly eradicated many diseases, saving millions of lives. Yet, in recent years, a dip in immunization rates—coupled with the proliferation of vaccine misinformation—has unleashed new debates about this critical public health measure.
Until recently, immunization rates have trended upward since their invention. Mid-century innovations were pivotal in developing vaccines: A combined vaccination for tetanus, diphtheria, and pertussis (whooping cough) was rolled out in 1948, followed by the polio vaccine in 1955. A vaccine for measles was first approved for public use in 1963. By 1971, it was combined with those for mumps and rubella to create the MMR vaccination.
The evolution of vaccination programs
Immunization advances dramatically lowered child mortality rates, with infant deaths decreasing by 40% worldwide over the past 50 years, according to a 2024 World Health Organization report. That's an estimated 101 million infant lives saved. "Vaccines are among the most powerful inventions in history, making once-feared diseases preventable," WHO Director-General Dr. Tedros Adhanom Ghebreyesus said in a statement.
It took more than just the invention of vaccines to see results, though. Public health campaigns and funding initiatives helped raise awareness about their importance, which increased vaccine accessibility. In 1962, President John F. Kennedy signed the Vaccination Assistance Act, designating government funds to ensure children under 5 received vaccines regardless of their family's income. In 1974, WHO launched the Expanded Programme on Immunization to ensure children across the globe have equal access to vaccinations.
Public health campaigns about vaccines were often created in response to crises. In the late 1980s, a measles outbreak prompted a national public health campaign to bring series 9 vaccines to public attention. Referring to the nine immunizations received by age 2 at the time, the campaign signs featured a cute baby and read, "We can think of 9 good reasons to vaccinate on time, but you need only one."
Addressing vaccine hesitancy and disparities
Despite substantial evidence backing the safety and efficacy of immunizations, protests against them date back to mid-19th-century England, when the British government mandated smallpox vaccinations. Objections varied over time. Some expressed concerns that the government should not have control over their bodies; others said vaccines conflict with their religious beliefs or expressed fears about their safety.
In November 2024, vaccine backlash again entered the public discourse when Robert F. Kennedy Jr. was nominated and later confirmed as Health and Human Services Secretary. Taking a position in direct contrast to that of his late uncle, Kennedy has been vocal in his skepticism of vaccines. He has perpetuated false claims that vaccines are linked to autism—a theory from a 1998 study that was retracted for inaccuracy soon after publication.
In 2019, on a trip to Samoa, Kennedy met with locals who were also against vaccinations. Just months after this visit, an outbreak of measles there killed 83 people, most of whom were infants and children. The Samoa outbreak is not unlike past outbreaks in the U.S., where gaps persist in vaccination rates among children who live below the federal poverty level. Coverage for childhood vaccines was also lower among the uninsured or those covered by Medicaid, according to Centers for Disease Control and Prevention data.
Northwell Health partnered with Stacker to explore how socioeconomic factors influence vaccination rates, using data from the CDC. Keep reading to learn more about the challenges children face in getting vaccinated and how these difficulties could be exacerbated in the coming years.
Systemic barriers limit vaccine access in kids under 24 months old
Current guidelines recommend that all children receive vaccinations to protect against 15 major illnesses by age 24 months. The CDC tracks most of these through the completion of the combined 7-vaccine series, a grouping of vaccines administered during the first two years of life that covers everything from polio and measles to hepatitis B. Although no states mandate vaccinations, children are required to receive their immunizations to attend public schools and many daycare centers.
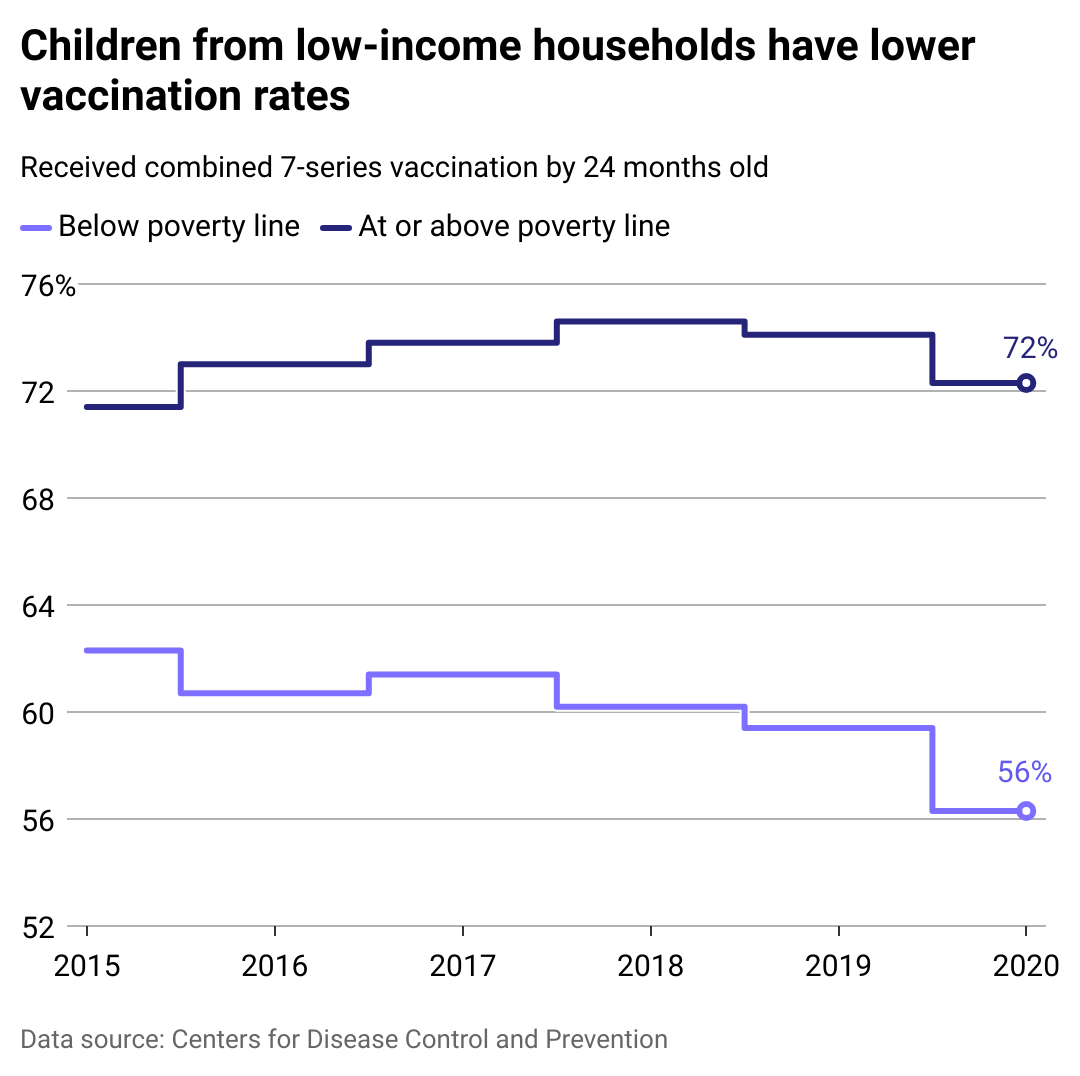
Children living below the poverty line receive the 7-vaccine series at a significantly lower rate than those who live above the poverty line, according to CDC data. This disparity has increased in recent years. While approximately 68% of all U.S. children born in 2020 received these critical vaccines by age 2, the completion rate was just over 56% for children who live below the poverty line—a notable decrease from the nearly 61% completion rate of those living below the poverty line who were born just five years earlier.
Vaccine completion rates are also higher among non-Hispanic white children, those with private insurance, and those living in urban areas.
Various factors contribute to these disparities, including income and insurance coverage. Those with lower incomes or who lack health insurance may be unable to afford the cost of office visits, even though the cost of vaccines themselves is covered—particularly at the frequency required within the first few years. Babies usually have 10 well visits in the first 24 months of life to monitor growth and administer vaccines on schedule.
Practical considerations can add more challenges. Those experiencing poverty tend to have less flexible work schedules, and they may lack transportation or live in more rural areas that are further from doctors' offices. Families living below the federal poverty level also tend to move more frequently, making it difficult to keep up with a paper trail of their vaccination history.
Furthermore, medical professionals' lack of cultural or language fluency to reach wider communities, and the health care system's lasting legacy of negative and exploitative practices have led to a deep-seated mistrust of doctors in some communities. The proliferation of incorrect or misleading information about vaccine safety and efficacy may further compound these practical barriers.
Recent drops in vaccinations are, in part, attributed to the COVID-19 pandemic, which halted and delayed routine doctor visits. Some children missed regularly scheduled vaccinations or received them late. Completion rates for the combined 7-vaccine series fell from approximately 70% for all children born between 2018 and 2019 to about 67% for kids born between 2020 and 2021.
Despite the impact of the VCF program, barriers to vaccination remain
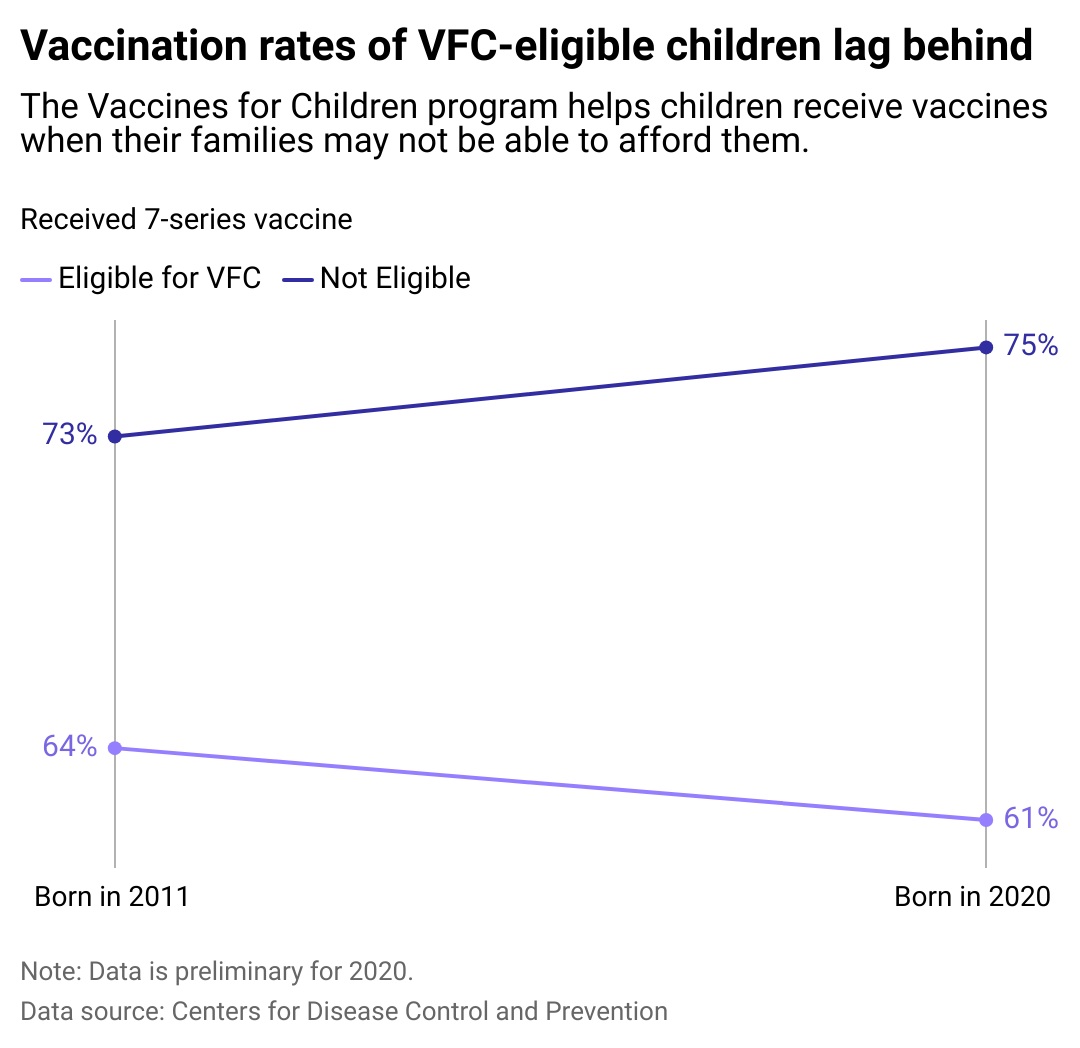
In 1994, Congress created the Vaccines for Children program following a series of measles outbreaks in the late 1980s and early 1990s. The VFC program provides free vaccinations to all children aged 18 and under who are uninsured, underinsured, eligible for Medicaid, or Alaska Native or American Indian. Prior to this, vaccines were covered only by insurance companies—or at a high out-of-pocket cost for those without health insurance. Thanks to the VFC, over half of U.S. children born in 2020 qualified for free vaccinations.
Although the CDC provides funding for over 60 programs that put the VFC program into action across the country, vaccination rates for those eligible remain much lower than the overall population—and this discrepancy grows each year. For those born in 2020, just 3 in 5 (61%) VFC-eligible children completed their 7-vaccine series, compared to 3 in 4 of those ineligible for the program. VFC-eligible kids face difficulties in completing vaccines that require multiple doses, as well as doses scheduled after the first year.
Despite ongoing challenges, the program has proven vital roughly 30 years since its launch. The CDC estimates vaccines have prevented 508 million illnesses between 1994 and 2023—saving not only lives but also out-of-pocket costs for parents and trillions of dollars in future health care costs by stopping the spread of serious diseases.
This could all change in the coming years, though. Concern in the medical community in response to Kennedy's plans for reforming the U.S. health care system. Although Kennedy denies intentions to completely abolish vaccinations, he has a clear history of speaking out against them, even saying there is "no vaccine that's safe and effective."
Concern about vaccine misinformation has ratcheted up since March 2025, when the ongoing measles outbreak began in West Texas and spread to neighboring New Mexico. As of early April 2025, the highly contagious diseases has already climbed to highest number of measles infections seen in a single year since 2019, during a wave of cases. The current outbreak has also claimed the lives of two children.
Kennedy has been vocal about cutting CDC funding, which oversees programs like the VFC. Though Kennedy has said he won't "take away anybody's vaccines," he has advocated for revoking approval for parts of the combined 7-vaccine series, arguing that further studies are needed, as well as increased parental choice.
Although the head of HHS cannot directly implement these plans, the role has the authority to appoint or replace members of the Advisory Committee on Immunization Practices. The head of the HHS role could also influence Kennedy to cut or reduce other initiatives, like the Section 317 program, which provides federal vaccine grants to state and local health departments.
Spike in kindergarteners receiving vaccine exemptions may threaten herd immunity
Immunization rates have been dropping prior to Kennedy's rise on the political stage, which began during the COVID-19 pandemic and was fueled by the spread of misinformation.
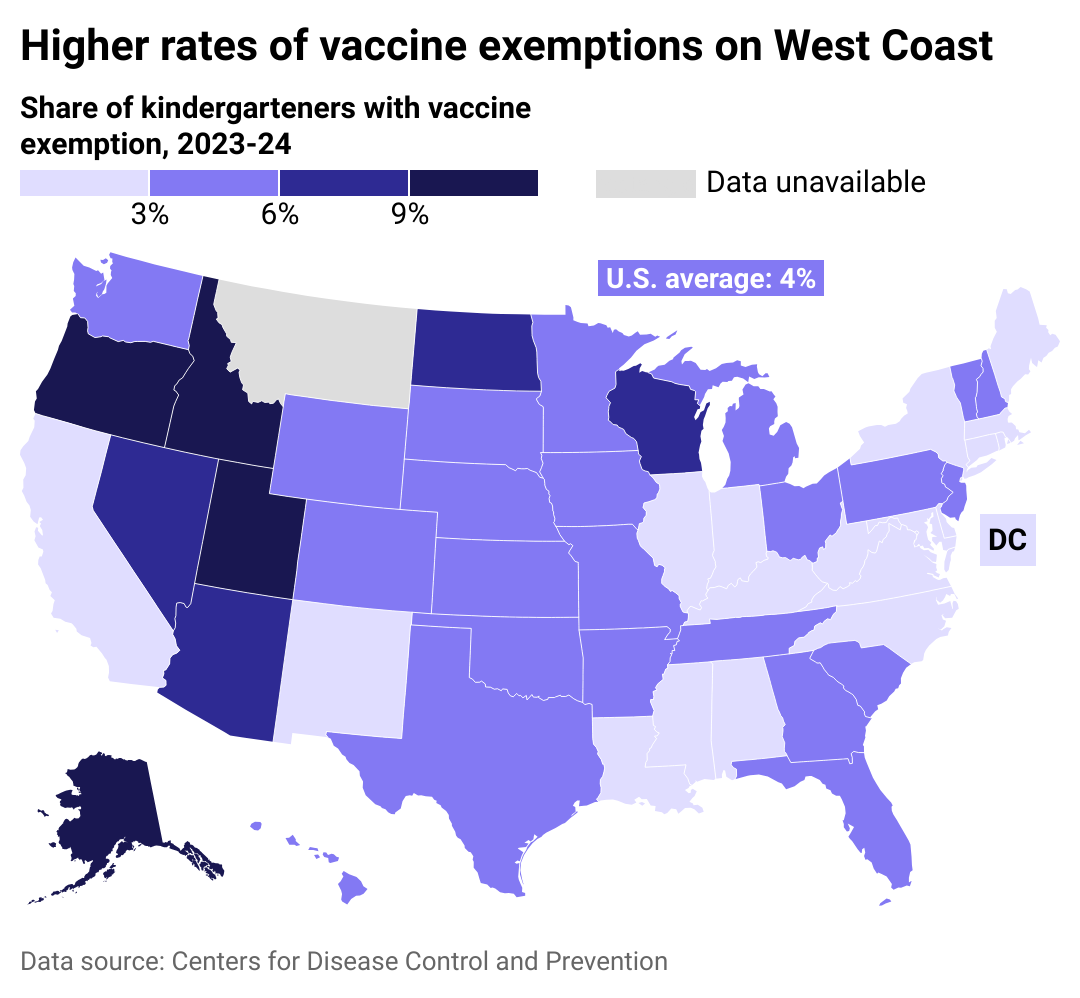
Although U.S. public schools require certain vaccinations before children can attend, each state allows medical exemptions, and most allow exemptions for religious or personal beliefs. While the share of kindergarteners with medical exemptions has remained steady at about 0.2%, the share of children with nonmedical exemptions has shot up.
During the 2023-2024 school year, an average of 4% of kindergarteners' families across the U.S. requested exemptions—more than double the 2011-2012 school year. The highest numbers were seen in Western states like Idaho, Oregon, and Alaska, with a rate well above average at 14.3%. Mississippi, California, New York, and West Virginia had the lowest exemption rates in the nation, with each under 1%.
Experts attribute rising exemptions to the surge of misinformation around vaccine safety and efficacy, particularly during the COVID-19 pandemic. According to a 2024 peer-reviewed study headed by a Columbia University researcher, negative messaging on social media and distrust in institutions have caused vaccine hesitancy at a difficult rate to mitigate. Coupled with political polarization and the spread of misinformation through mass media, the potential impact on the understanding of vaccines is significant.
While an average of 4% may seem like a small portion of the population, childhood vaccines are a public health measure. If enough kids in a particular school or community are vaccinated, the group can benefit from herd immunity, which helps prevent those who are unvaccinated from contracting a disease. However, viruses like measles are so easily transmitted that 95% of a community must be immunized to prevent the spread of disease.
When children with vaccine exemptions cluster—often in more affluent areas, around private schools—this creates favorable conditions for an outbreak. Evidence of the effects of decreased vaccination rates was seen toward the end of 2024, with cases of measles and whooping cough reaching the highest levels in five years.
At least 3 in 4 parents surveyed support school vaccine requirements; however, nearly 2 in 5 (38%) parents seeking exemptions did so based on personal or philosophical beliefs, not medical reasons. A 2024 parent survey conducted by the CDC showed that while about a third of parents believed unvaccinated children should be able to attend school, over half agreed those children should stay home during an outbreak.
Contracting these illnesses can significantly impact not only a child's physical health but also lead to them missing school and falling behind academically or socially. Continued intervention is necessary to ensure the safety of all children, especially higher-risk populations like those experiencing poverty.
With the resurgence of diseases once under control or even eliminated (meaning there was no new spread of disease over a 12-month period), some states have become more stringent about exemptions. New York disallowed religious exemptions following disease outbreaks, and California implemented a policy that requires parents seeking vaccine exemption to first be educated on the risks. While this hasn't produced much change among private school students, those living below the poverty level have shown a greater decrease in exemptions.
It's important to note the distinction between families who don't complete their childhood vaccinations due to systemic barriers and those who abstain by choice. Ultimately, however, they'll face the same consequences. Any unvaccinated child will be more susceptible to the spread of disease and its painful and, in some cases, debilitating consequences.
Yet it's the children below the poverty line—uninsured, underinsured, and often facing obstacles merely to get to the pediatrician for their MMR shot—who will inevitably pay a greater price.
Data reporting by Tory Lysik. Story editing by Alizah Salario. Copy editing by Janina Lawrence. Photo selection by Ania Antecka.



