Older Black people die at higher rates than their white peers. Here's why aging is a greater risk for Black Americans.
This story originally appeared on QMedic and was produced and distributed in partnership with Stacker Studio.
Older Black people die at higher rates than their white peers. Here's why aging is a greater risk for Black Americans.
For older Black people in America, the golden years often come with a harsh reality: They are more likely to suffer from chronic illnesses, be sicker in old age, and die younger than their white counterparts.
In 2018, Black Americans' average life expectancy was 74.7 years, four years less than the overall average of 78.7. However, a drop in life expectancy during the COVID-19 pandemic further exacerbated racial disparities among mortality rates: Black people were expected to live 70.8 years, compared with 76.4 years for white people and 77.7 years for Hispanic people, according to 2021 provisional data.
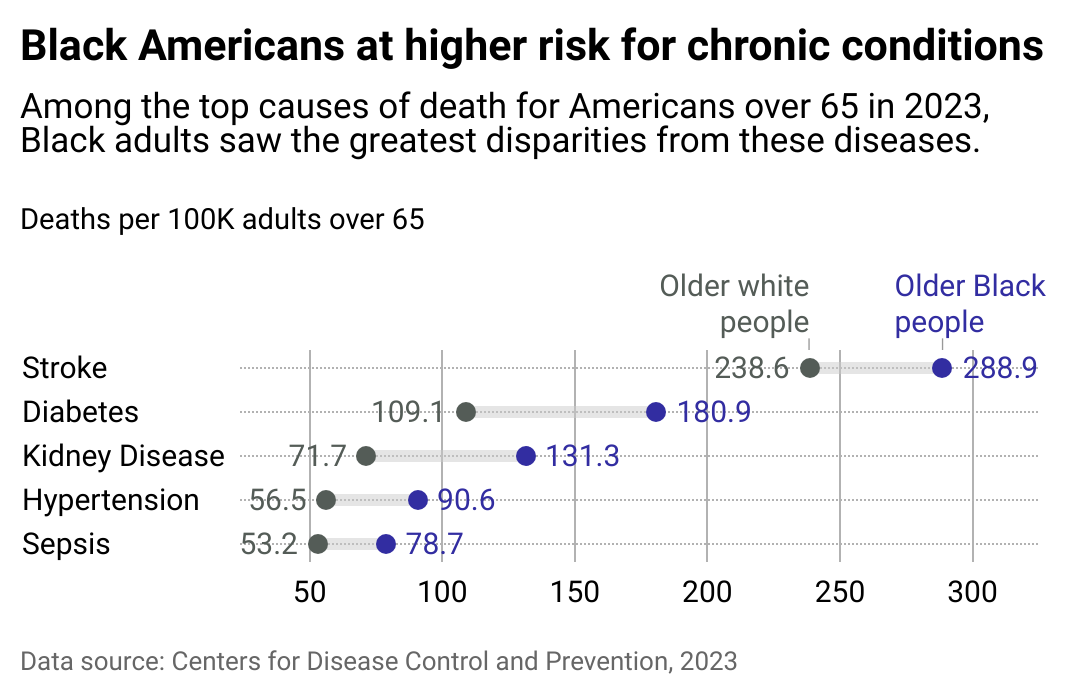
Black Americans were also 20% more likely to be diagnosed with high blood pressure and 1.4 times more likely to be diagnosed with diabetes than non-Hispanic white adults, according to 2025 data from the Department of Health and Human Services Office of Minority Health. They also tend to have worse outcomes and higher mortality rates for cancers, including lung and prostate cancer. Recent data from the CDC shows older Black populations die from stroke, diabetes, kidney disease, hypertension, and sepsis (a life-threatening reaction to an infection) at significantly higher rates than their white peers.
Research has shown that Black people encounter worse health outcomes as they age due to a lifetime of unequal access to health care, healthy food, safe housing, and economic opportunities. These nonmedical factors influencing health and well-being are known as social determinants of health, according to the Centers for Disease Control and Prevention.
Social determinants of health often amplify with age. "We are living in bodies that have to endure multiple harms that attack us throughout the life course," Dr. Jessica Owens-Young, associate professor of health studies at American University, told Stacker. "When we finally reach the age of being a senior, all of those experiences can lead to entering seniorhood or eldership—those golden years—with a body and with experiences that have been weathered."
QMedic analyzed data from the CDC and spoke with experts to take a hard look at the reality of aging as a Black person in America.
Carrying a lifelong burden of racism and ageism
The harms experienced by Black people are well documented: The majority (75%) of Black adults say they've experienced racial discrimination either regularly or occasionally, according to Pew Research Center. Black Americans are statistically more likely than whites to have experienced the death of an immediate family member before midlife, an often overlooked source of stress and trauma. These types of consistent physical and psychological stressors contribute to what's known as the allostatic load, or chronic stress that accumulates in the body, which exacerbates numerous health issues, including poor appetite or overeating, frequent headaches and stomachaches, and alcohol and substance abuse issues—all of which are more common among Black Americans.
For older Black people, this means that the natural effects of aging are accelerated. The additional "wear and tear" is a phenomenon known as "weathering," first introduced by public health researcher Dr. Arline Geronimus. It illustrates how, for older Black people, prolonged exposure to stress and adversity can accelerate the aging process, leading to the earlier onset of chronic health issues.
Researchers at the Mayo Clinic and elsewhere found that Black Americans had a biological age nearly 12 years older on average than their chronological age. In comparison, their white counterparts had an average biological age that was 10 years younger than their actual age. In other words, Black Americans weather 6.1 years faster than their white counterparts.
Medical experts note that social determinants include policies that determine or limit access to housing, education, and economic opportunities, all critical to long-term health. For example, redlining, a practice where lenders assess financial risk based on property values and a property owner's race and ethnicity, continues to harm communities of color more than 50 after the 1968 Fair Housing Act made redlining illegal, according to the University of California, Berkeley, School of Public Health. ZIP codes corresponding to formerly redlined neighborhoods were shown to have higher rates of COVID-19, according to a study from the IZA Institute of Labor Economics.
Formerly lower-grade D neighborhoods, which had higher portions of non-white residents, were close to nearly twice the density of oil and gas wells compared to higher-grade A neighborhoods. Women's reproductive health was also affected with more associations to low birth weight and preterm births in these historically redlined areas.
"Systemic barriers and misdiagnoses are rampant, even with resources; without an advocate, navigating the health care network can be nearly impossible," Dr. Ryon Cobb, a professor of social work at Rutgers University, told Stacker. Many Black people live in health care deserts, according to Cobb, where they do not have access to information or even doctors with the expertise to provide treatment.
The intersection of ageism and systemic racism compounds is often called a "double disadvantage" for older Black people, according to the American Geriatrics Society. This means navigating a health care system that often overlooks their specific needs, from implicit biases in diagnostic practices to underrepresentation in clinical trials.
The impact of discriminatory practices and mistrust heightens with age
Reliable transportation, an often overlooked barrier, plays a significant role in health disparities, especially among older Black populations. Urban Institute data from 2022 found that 8% of Black adults missed or delayed medical care due to transportation issues, compared to 4% of white adults. Another major compounding factor is inadequate health insurance coverage. Black beneficiaries comprise just under 11% (6 million) of the U.S. Medicare population, though they account for a disproportionate number in some states. In Mississippi, for instance, Black beneficiaries account for 31% of total Medicare recipients, and in Washington, D.C., that number surges to 63%. Notably, Black Americans have a lower life expectancy after age 65 than their white or Hispanic counterparts.
The importance of transportation was recognized in 2021, when transportation services for nonemergencies were included on a list of mandatory benefits for people with Medicaid who lack reliable modes of travel. A growing number of Medicare Advantage plans now include this benefit.
Historical discriminatory practices within the medical system have also been well-documented throughout history, and this legacy also plays a role. Some 7 in 10 Black Americans say they've received unfair treatment by the health care system, and over half (55%) say they distrust it. Black adults are more likely than whites to report they have to be careful about their appearance to be treated fairly by health practitioners, and that a health care provider has refused them prescription pain medication they thought they needed, according to 2024 KFF data.
These types of negative experiences and unfair treatment contribute to a persistent lack of confidence in the system. This can heighten mistrust and discourage seeking preventative care, according to a 2024 qualitative study of 25 Black patients discharged from emergency room departments published in JAMA Health Forum.
Study participants reported experiencing dismissiveness and a lack of confidence in their health literacy, making them hesitant to seek medical attention. That, in turn, can exacerbate existing conditions and delay diagnoses.
As one study participant put it, "seeking health care for a Black person is a roll of a dice all the time. [There will never] be a moment at this time in [the US] that a person of color [is] like, 'Oh, I'll just go to the doctor.' No, it'll be…'Okay, what doctor am I going to? Is it bad enough that they'll treat my condition [seriously], or should I wait until it's bad enough that they have to?' That's a terrible way to live, and that's how we live. We show up in the emergency room because everything else gets dismissed…so it gets bad enough that [there's] no other choice until we have to get treated…it's terrible."
Chronic kidney disease, for example, often goes undiagnosed among Black communities, according to Cobb. Yet Black Americans are more likely to progress to end-stage kidney disease: Without tailored interventions that address both systemic racism and ageism, these health disparities can continue to widen, posing the same risk to future generations.

What's being done to curb disparities
Grassroots organizations nationwide can be crucial for empowering older Black populations to take control of their health. "Fundamentally, we must return to our ancestral tradition of treating aging as a collective rite of passage and not as an individual test of mettle," Carlene Davis, co-founder of Sistahs Aging with Grace & Elegance, told Stacker.
In California, the California Black Women's Health Project collaborates with Sistahs Aging with Grace & Elegance to host "Celebrating the Aging Journey" seminars, which support Black women in planning for long, healthy, and financially secure lives while also providing resources for caretakers of older people.
Healthier Black Elders Center in Detroit works to reduce health disparities through research and education. HBEC offers health education workshops and screenings and maintains a Participant Resource Pool to encourage research participation among older Black adults. Its goal is to increase the representation of older Black adults in research, as this demographic has historically had a low participation rate.
In communities across the country, companies like Uber Health have partnered with health care organizations to offer rides to medical appointments for older people. The partnership aims to reduce missed appointments, allow for more consistent care, and, ultimately, improve health outcomes.
On a national level, the Diverse Elders Coalition represents older people throughout the country: American Indians and Alaska Natives, Asian Americans, Pacific Islanders, Native Hawaiians, Black Americans, Hispanic and Latino Americans, and LGBTQ+ Americans. The coalition advocates for policies that improve aging outcomes for racially and ethnically diverse communities, addressing health disparities, economic security, and culturally competent care.
The National Caucus and Center on Black Aging also offers a health and wellness program that provides virtual events and newsletters tailored to older Black Americans.
Investing in culturally competent care
While the numbers are discouraging for older Black adults, efforts underway that center Black health also offer a glimmer of hope. "Black seniors fare better when they have Black or culturally competent and responsive health care providers. And far too often that is not the case," Davis said.
Research from the Georgetown University Health Policy Institute confirms this, and recommends that providers and organizations implement culturally competent practices to enhance the quality of care. These practices include offering interpreter services, recruiting and retaining diverse staff, and providing training in cultural awareness, knowledge, and skills.
A 2020 study of low-income patients with heart failure who lived on the South Side of Chicago published in the journal Critical Pathways in Cardiology found that those who received weekly visits from a community health worker had a 75% decrease in emergency visits due to heart failure and an 89% decrease in heart failure-related readmissions, as well as a significant reduction in costs related to the disease.
The importance of culturally competent care extends beyond community programs. A 2022 study of 1,618 U.S. counties published in JAMA Network Open found that every 10% increase in Black primary care representation was associated with a higher life expectancy of about 31 days. Higher representation levels were also associated with lower death rates due to any cause and even lowered the mortality rate disparities between Black and white patients.
Over time, higher mortality rates coupled with excess deaths among the Black population have accumulated. In a study led by researchers at the Yale School of Public Health, 80 million years of potential life were lost among Black Americans over the course of two decades. Those are years, and lives, that they won't get back.
Story editing by Carren Jao. Copy editing by Janina Lawrence.