
What nervous system dysregulation actually means, according to therapists
What nervous system dysregulation actually means, according to therapists
Your heart races during a normal work meeting. A friend’s offhand comment replays in your mind for days. You feel exhausted but can’t sleep, or you’re going through the motions but can’t quite feel present. If these moments sound familiar, you might be experiencing what’s become one of the most discussed topics on social media: a dysregulated nervous system.
The term is everywhere right now, and for good reason: It captures something many people are experiencing but haven’t had language for. In this article, Thriveworks breaks down what nervous system dysregulation actually means, why it happens, and most importantly, what you can do about it.
What is a dysregulated nervous system?
Having a dysregulated nervous system means your body’s stress response is out of balance. It’s chronically overreacting or underreacting, to the point where it’s interpreting benign triggers or situations as potentially harmful to your mental, emotional, or physical well-being.
“You’re in a mode where everything is a threat,” says Alexandra Cromer, a licensed professional counselor and lead clinician at Thriveworks.
To understand why this happens, it helps to know how your stress response is supposed to work. Your autonomic nervous system includes your sympathetic nervous system (fight or flight) and your parasympathetic nervous system (rest and digest). In harmony, these two systems help you swiftly respond to danger and then return to baseline once the threat is gone.
For example, your body physically and mentally amps you up to run out of a burning building—your heart rate spikes, adrenaline floods your system, your muscles tense—and then calms you down once you’re safe so you can focus on recovering as your heart rate slows and cortisol levels drop.
In a dysregulated state, “you’re in survival mode,” says Kerry Green, LCSW, a therapist who specializes in anxiety and trauma. Your innate survival mechanisms work against you by causing mental, emotional, or physical symptoms that feel more overwhelming than protective—no burning building required. This happens because your nervous system has learned to perceive threats where none exist, often due to past experiences that have trained it to stay on high alert.
Signs of a dysregulated nervous system
A dysregulated nervous system can cause a wide range of symptoms. Think of your nervous system as having a “window of tolerance”—a zone where you can handle daily stressors without tipping into overdrive or shutting down. When you’re inside this window, you feel reasonably in control of your thoughts and emotions, even when life gets stressful.
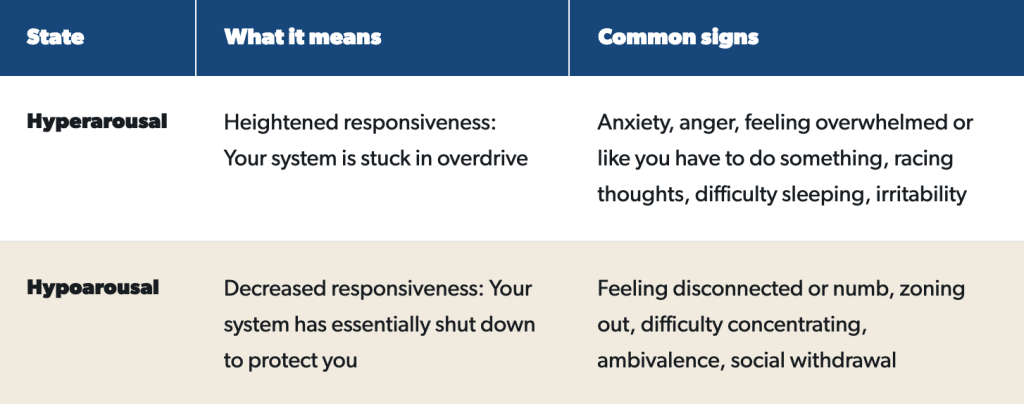
When you fall outside the window of tolerance, symptoms generally fall into one of two buckets: hyperarousal (overreactions or heightened responsiveness) and hypoarousal (underreactions or decreased responsiveness).
Hyperarousal vs. hypoarousal: A quick comparison
Hyperarousal may look and feel like:
- Persistently feeling on guard or alert
- Chronic worrying, rumination, or disturbed sleep
- Exaggerated startle response
- Fast or irregular heart rate
- Shallow or irregular breathing
- Sweating
- Muscle tension
- Digestive issues tied to stress
- Pleasing others by overcommitting or seeking validation
- Anger, irritability, or snappiness
Hypoarousal may look and feel like:
- Persistently feeling low energy or sluggish
- Going through the motions
- Zoning out frequently
- Dissociation (feeling disconnected from your body)
- Difficulty concentrating or making decisions
- Can’t do anything or don’t feel like yourself
- Self-isolation or social withdrawal
- Feeling hopeless or depressed
- Pleasing others by neglecting personal needs
- Numbness or emotional disconnection
Important note: Experiencing any of these symptoms occasionally is normal, especially during periods of high stress. Fight, flight, freeze, or fawn (also known as people-pleasing) should be temporary states of dysregulation, with your parasympathetic response eventually taking over and calming your body down once you feel safe.
When it might be a problem: You’ll skew toward chronic dysregulation when one or more of these symptoms become a frequent, persistent, or baseline response, particularly when you’re having a hard time anticipating triggers or you’re not facing an obvious threat to your well-being.
What causes nervous system dysregulation?
Your nervous system uses what you’ve experienced in the past to interpret what’s happening in the present. “Every second, it is wondering, ‘What does this remind me of? Oh, that sounds like my dad, who used to criticize me all the time,’” Green explains. “Your nervous system doesn’t just want to protect you from [physical] danger. It also wants to protect you from [emotional] pain.”
Here are some of the most common reasons it gets stuck in defense mode.
Trauma, big or small
Trauma is a well-known driver of a dysregulated nervous system. In fact, signs of hyperarousal or hypoarousal are part of the criteria for a post-traumatic stress disorder diagnosis.
“Big T” traumas include things like physical or sexual assault, a loved one’s death, or surviving an accident or natural disaster. “Little T” traumas encompass experiences like job loss, chronic illness, or being bullied or heavily criticized as a child. Either can lead to changes in brain activity that can then alter how your nervous system responds to perceived threats.
Chronic stress from modern life
The grind of modern life can dysregulate your nervous system, in part because it keeps you on high alert. Seemingly endless notifications, rising political and cultural tensions, steady social commitments, financial stressors, and caregiving responsibilities can pile up and push your limits. “You may think burnout is your fault, but it’s not,” says Kate Hanselman, a psychiatric mental health nurse practitioner at Thriveworks. “It’s part of working in a system that doesn’t serve you.”
Chronic depression or anxiety
Ongoing depression or anxiety also triggers frequent fight, flight, freeze, or fawn states, keeping your stress response perpetually activated. Depression often pulls you into freeze or shutdown mode, while anxiety tends to keep you in flight or hypervigilance—and being stuck in either state for too long can tip you into the other.
Neurodivergence
ADHD, autism, and other forms of neurodivergence can also be characterized by dysregulation, Hanselman says. This includes hyperarousal (sensitivity to noise or light, emotional fluctuations) and hypoarousal (difficulty focusing, social withdrawal) due to differences in brain functioning.
Disturbed childhood attachment
Chronic stress or trauma that’s linked to a lack of safety and secure “attachment” to caregivers—say, due to emotional neglect—can influence brain development during these formative years, setting the stage for a more reactive nervous system later on. These “inner child” wounds often surface in adult life as heightened sensitivity to rejection or difficulty trusting people.
How to regulate your nervous system
There are dozens of practical and science-backed ways to start regulating your nervous system on your own. While each self-regulation technique looks a little different, they’re all centered on getting you closer to rest-and-digest mode when symptoms like racing thoughts, muscle tension, or emotional numbness start to flood in.
They also require practice: You shouldn’t over-exercise to “burn off” stress, sprint away from your triggers, or force yourself to relax when you can’t. Start with one or two techniques and, like a muscle, build them up over time. Here’s what experts recommend.
1. Lay a solid foundation with basic self-care.
It’s not that exciting, but the most basic things often make the biggest difference. Exercising regularly, eating well and enough, staying hydrated, and prioritizing sleep are nonnegotiables. If you don’t give your body what it needs to physically function, then you’re probably going to struggle mentally and emotionally, Cromer says.
2. Build predictability with simple routines.
Your nervous system hates surprises, Green says. Give it the predictability it craves with steady morning and night routines. Start with just one or two consistent habits, like waking up and falling asleep around the same time, blending a smoothie in the morning, and applying your skincare before bed at night.
3. Create distance from triggers when you can.
It’s not realistic to completely avoid the triggers that set you on edge. Instead, do your best to calm your mind and body when your environment is overwhelming your system, Hanselman says. Briefly walk away from an argument to compose yourself, put on headphones if a screaming child is stressing you out, or gently close your eyes if you need a break from harsh lights, for example.
4. Try vagus nerve stimulation exercises.
Your vagus nerve is the longest nerve in your body, running from your brain to your gut. It plays a key role in your parasympathetic response, or your “rest and digest” functions (including your breathing patterns, heart rate, and digestion speed). Stimulating your vagus nerve—say, by breathing deeply, dipping your face into cold water, or humming—tells your body to relax. With consistent practice, these exercises act like a recovery toolkit.
5. Find the right movement for your body.
Some people feel better when they do gentler movements like yoga, others prefer intense workouts like running or boxing, and research suggests rhythmic activities like dancing can set the spark for your parasympathetic response. The key is to do whatever feels best to you consistently, because regular movement helps you stay regulated versus having to get regulated, Hanselman says.
6. Protect your downtime like an appointment.
Block out intentional rest time on your calendar, then fill it with something that feels particularly nourishing to you, whether that’s a warm soak in the tub or a movie night with your favorite snacks. Especially if you’re under high stress or feeling burnt out, carving out intentional time to rest gives you the real and perceived sense of control your nervous system craves, Cromer says.
When to seek professional help
The above strategies can quell in-the-moment symptoms and help you feel less reactive over time. But if your symptoms persist and are messing with your quality of life—including your ability to take care of yourself emotionally and physically, tend to your relationships, and show up in the way you’re expected to at work—it’s time to connect with a mental health professional.
A licensed therapist can help you unpack the root causes of your nervous system dysregulation and guide you on the most appropriate path forward for your needs. If you’re struggling with trauma, for example, they may refer you to an EMDR specialist. If inner child wounds are the culprit, they may use a modality called internal family systems. They may also refer you to a psychiatric provider to discuss whether medication might be right for you.
This story was produced by Thriveworks and reviewed and distributed by Stacker.



