30 things we've learned about COVID-19 since January
30 things learned about COVID-19 since January
Since the initial outbreak, much has been learned about COVID-19. It's also known that spreading wrong information is dangerous and does little to help flatten the curve and contain the coronavirus. New information on COVID-19 is released daily, but some facts about the virus and its disease remain true.
Stacker used compilation articles in STAT and Scientific American to pull together a list of findings summarizing the current state of scientific knowledge on the coronavirus and the disease it causes. The findings in this story come from the Centers for Disease Control and Prevention, scientific papers, and credible news organizations.
It's still true that some fundamental practices can help stop the spread of the coronavirus, including mask-wearing, social distancing, and sanitizing, but some lesser-known facts also warrant attention. Women tend to fare better when contracting the virus than men, race plays a significant role in who survives the virus, and people over 60 are more at risk for becoming very ill. People with underlying conditions are also more vulnerable to the coronavirus. Yet, there are still many things that researchers do not know about it and continue to search for answers.
It can be challenging to keep up with the spread of information about the coronavirus. Scientists learn new things about it daily, which is why Stacker has taken the time to break down some of the more essential facts. It has included linked resources and details and data from reputable sources so you can read more about particular studies and understand some slides in more detail.
Scientists have been working on a vaccine for COVID-19 for months, and many of those options are now in the human trial phase. While the world waits for this vaccine, understanding the virus and how to prevent its spread is vital.
Read on to learn more about the coronavirus and COVID-19. Know the facts.

The coronavirus most likely originated in bats
At the start of the pandemic, it was believed that the coronavirus primarily originated in bats. The current hypothesis is that the virus did originate in bats, but then jumped to humans through pangolins. The precise route of transmission is not yet known.

Only one major strain of the coronavirus has been identified
While widely assumed, alternate strains of the coronavirus have not been identified. The coronaviruses do not mutate rapidly, and only one strain, or genetic sequence, of the virus has been found.

The coronavirus primarily spreads through the air
Sanitizing surfaces is essential in trying to stop the spread of the virus, but the coronavirus is predominantly spread through the air, making an emphasis on ventilation more crucial than surface cleaning. It’s been found that poorly ventilated spaces can be a breeding ground for the coronavirus.

Contaminated surfaces are still a concern
The coronavirus spreads more rapidly through the air than through surface touch, but contaminated surfaces can still cause infections. High-touch surfaces, such as door knobs, light switches, and faucets should be cleaned regularly in any setting.

People without symptoms can spread COVID-19
People with no symptoms of COVID-19, or with very few symptoms of it can quickly and effectively spread the virus. These people may be superspreaders. The term "asymptomatic" about COVID-19 is a misnomer as all people that contract the virus have symptoms—and could be considered "presymptomatic"—not being sick enough to seek medical attention.

Outdoor gatherings can be safe
Outdoor activities such as exercise, including walking, running or biking, and playing golf or tennis, are safer than indoor gatherings. While this may be the case, social distancing, mask-wearing, and sanitizing methods should remain intact whether inside or outside to prevent the spread of the coronavirus.

The coronavirus spreads quickly in communal living facilities
The coronavirus spreads rapidly in communal living spaces such as retirement homes and prisons. In the United States, 42% of deaths have been in long-term care facilities. “Nursing homes have been ground zero for COVID-19,” said Seema Verma, administrator of the Centers for Medicare and Medicaid Services.

Loud talking and singing spread virus more
People who talk loudly and those who sing in choirs tend to spread the coronavirus more often than people who do not. Mask-wearing can prevent the spread of the larger droplets emitted into the air by loud talkers and singers.

Superspreader events disproportionately drive outbreaks
Superspreader events are responsible for spreading COVID-19 on a large scale. Big crowds, close contact, and poorly ventilated spaces spur the spread of COVID-19 during superspreader events. It’s been reported that 80% of the spread of COVID-19 is caused by 10% to 20% of the infected people present at superspreader events.

Children are less likely to contract and spread the coronavirus
When it comes to the coronavirus and young children, they are more likely to be asymptomatic, but can still spread COVID-19 to both adults and other children. It is evident that infected children can have milder cases of COVID-19 than adults, and it's been determined that death or severe illness risks remain low.

Some children exposed to COVID-19 get very sick with MIS-C
Some children exposed to COVID-19 contract multisystem inflammatory syndrome (MIS-C) after being around someone with COVID-19 or contracting it. Most children that develop MIS-C are Hispanic/Latino or non-Hispanic Black. Symptoms include inflammation of body parts, including the lungs, heart, and brain, though this is not inclusive. Children may also have a fever and other symptoms such as fever and neck pain.

No summer letup for the coronavirus
The coronavirus is not impacted by heat or warmer weather. Summer months or humid climates do not result in a smaller number of cases or a slower spreading of COVID-19. Mask-wearing, social distancing, and sanitizing efforts should still be practiced, regardless of the weather.

There are no symptom standards for COVID-19
There are a myriad of symptoms that can indicate if someone has contracted COVID-19, ranging from fever to loss of smell to coughing or dizziness, and all present at various severities. No one standard set of symptoms exists for the coronavirus.

COVID-19 symptoms usually show up within two weeks
People with COVID-19 do not see symptoms for 2 to 14 days after being infected. Some signs to watch out for include fever, cough, sore throat, and severe trouble breathing. Some people may have mild symptoms, while others may require immediate medical attention.
Those with mild infections can spread the virus for up to 10 days
People with mild or moderate cases of COVID-19 can remain infectious up to 10 days after contracting the illness. People with severe cases can stay infectious up to 20 days, and those who recover can still spread the virus up to three months, though in smaller doses.

Symptoms can persist for months
People who survive a COVID-19 infection are known as long-haulers, and many of them do not feel as though they have fully recovered for weeks after the initial infection. The reason why symptoms can persist for months is unknown.

The disease may cause lasting damage
Lingering effects of COVID-19 can cause lasting damage. The heart, lungs, nervous system and other organs can all be impacted for an extended period.

Veklury (remdesivir) helps patients with COVID-19
Studies have shown that the antiviral drug Veklury (remdesivir) can help patients with severe cases of COVID-19. On Aug. 28, the U.S. Food and Drug Administration approved an emergency use authorization that broadens the scope for the use of Veklury to all people hospitalized with COVID-19 regardless of disease severity.

Older adults are more vulnerable to COVID-19
Elderly adults are more likely to contract a severe case of COVID-19 than younger people. The immune system becomes weaker as people age, resulting in greater vulnerability. People over 65 are particularly vulnerable to COVID-19.

Men are more vulnerable to COVID-19
The female immune system is more robust due to estrogen hormones, but there are other reasons why men are more susceptible. Some reasons men contract COVID-19 more often than women include more underlying conditions, worse overall health, and a difference in genes.

Racial disparities leave people of color more vulnerable
Race plays a large part in contracting COVID-19. More than twice the number of Black Americans have died from COVID-19 than white people. The reasons for this are multifaceted, including less personal space, essential worker occupations, less access to medical care, racism within the medical system, and lower overall health.

Underlying health conditions worsen COVID-19 outcomes
Underlying conditions such as heart disease, diabetes, and chronic lung disease worsen COVID-19 symptoms resulting in a bleaker outcome for patients. With already diminished lung or heart capacity, COVID-19 can be fatal to someone with a pre-existing condition.

Climate change exacerbated the pandemic’s impact
The air individuals breathe has a direct impact on their ability to fight infections, including COVID-19. Harvard researchers have found that people who live in an area with low air quality due to pollution are more likely to die from COVID-19. Air pollution can lead to respiratory problems making battling COVID-19 even more difficult.

Masks hinder the virus’ spread
Face masks block respiratory droplets. Wearing a face mask in public can help prevent the contraction of COVID-19 and from spreading it to other people. Studies in nearly 200 countries showed that death rates were lower if government agencies promoted mask-wearing.

Lockdown orders can help flatten the curve
Global lockdowns helped governments flatten the COVID-19 curve. Preventing mass gatherings and closing large buildings helped stop people from getting seriously ill.

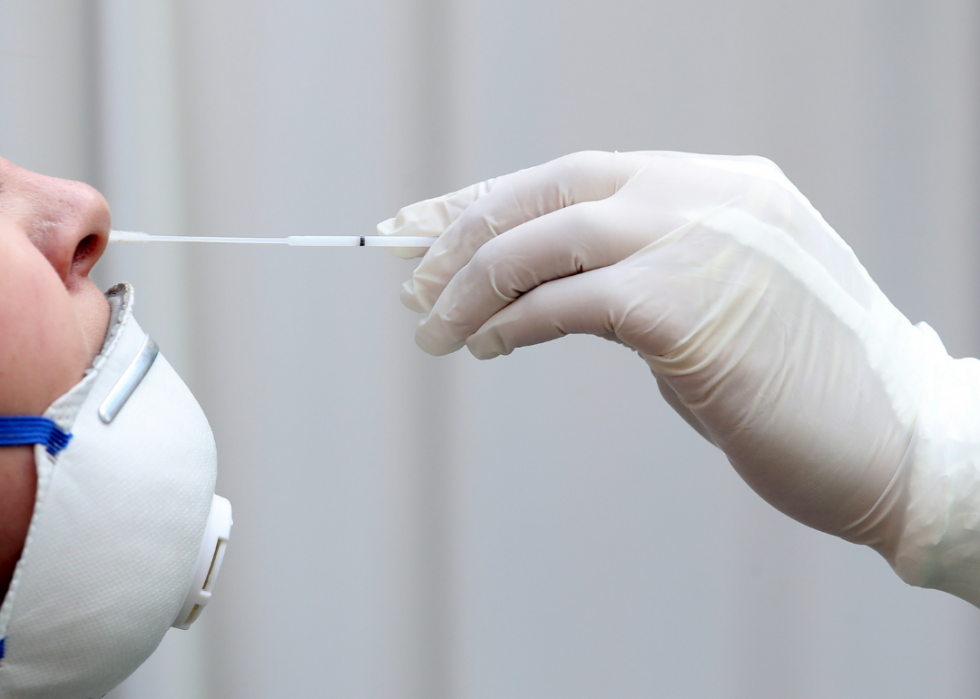
Widely available testing and tracing can help flatten the curve
Widely available tests can help flatten the coronavirus curve. San Francisco employed a free non-referral drive-through testing option for city residents and effectively contained the spread of COVID-19.

Clear communication can help flatten the curve
The way that governments communicate with the public can help flatten the curve. Communication should be precise and transparent without overpromising. In the United States, the Centers for Disease Control and Prevention is coordinating communication with employers to ensure that businesses know what is needed for effective COVID-19 control.

Misinformation is dangerous
Misinformation can kill when the incorrect details are rapidly spread. It’s vital to obtain information on the pandemic from reputable sources. Without a cure for COVID-19, it’s vital that experts be able to provide the public with clear, factual information about the disease.

Vaccine development can happen at "warp speed"
Vaccine trials for the coronavirus can be developed quickly because it is a virus scientists are familiar with; it is an acute virus; and scientists are employing new, faster, technology. Many potential vaccines are currently in Phase 3 trial—human trials—and they may be approved in months.

Reinfection is possible, but more study is needed on its implications
Some people initially infected with COVID-19 have been reinfected, but this may not happen to everyone who has tested positive for it. A second infection can also be a unique infection. More research is needed to confidently state that all people can be reinfected.