
Chronic pain is extremely common. What is it, and why is it so hard for many Americans to get relief?
This story originally appeared on Compare Inpatient Rehab and was produced and distributed in partnership with Stacker Studio.
Chronic pain is extremely common. What is it, and why is it so hard for many Americans to get relief?
Muscle and joint aches. Shooting, stinging, or burning pain. Ongoing stiffness or squeezing sensations, pain so persistent and intense that it leads to constant fatigue, anxiety, depression, and insomnia.
These and other symptoms of chronic pain are often associated with older adults, but chronic pain is a pervasive public health issue that is hard to measure. Nearly 1 in 4 adults said they experienced chronic pain, according to a 2023 survey by the Centers for Disease Control and Prevention. Almost 1 in 10 reported that their daily life or work had been impacted by persistent, debilitating pain in the past three months. On top of the personal toll that chronic pain takes on Americans, the financial cost to the country of health care expenses and lost productivity can exceed hundreds of billions of dollars annually.
The U.S. Pain Foundation describes chronic pain as an "epidemic hiding in plain sight." However, quantifying how many people are affected is difficult since available data relies on patients self-reporting how much pain they experience, which is subjective. This subjectivity also makes it difficult to measure the impact of chronic pain on people's daily lives and limits the chance federal health policies will prioritize this condition.
Compare Inpatient Rehab examined data from the CDC's National Health Interview Survey to examine the chronic pain epidemic and what is behind it.
Chronic pain is the most common reason that people seek medical care. However, people living with high-impact chronic pain—pain that limits daily activities on all or most days for three months or more—experience more substantial mental health issues and chronic impairments. HICP often restricts activities like work, social, and self-care, generating a sense of helplessness or a constant fear of pain.
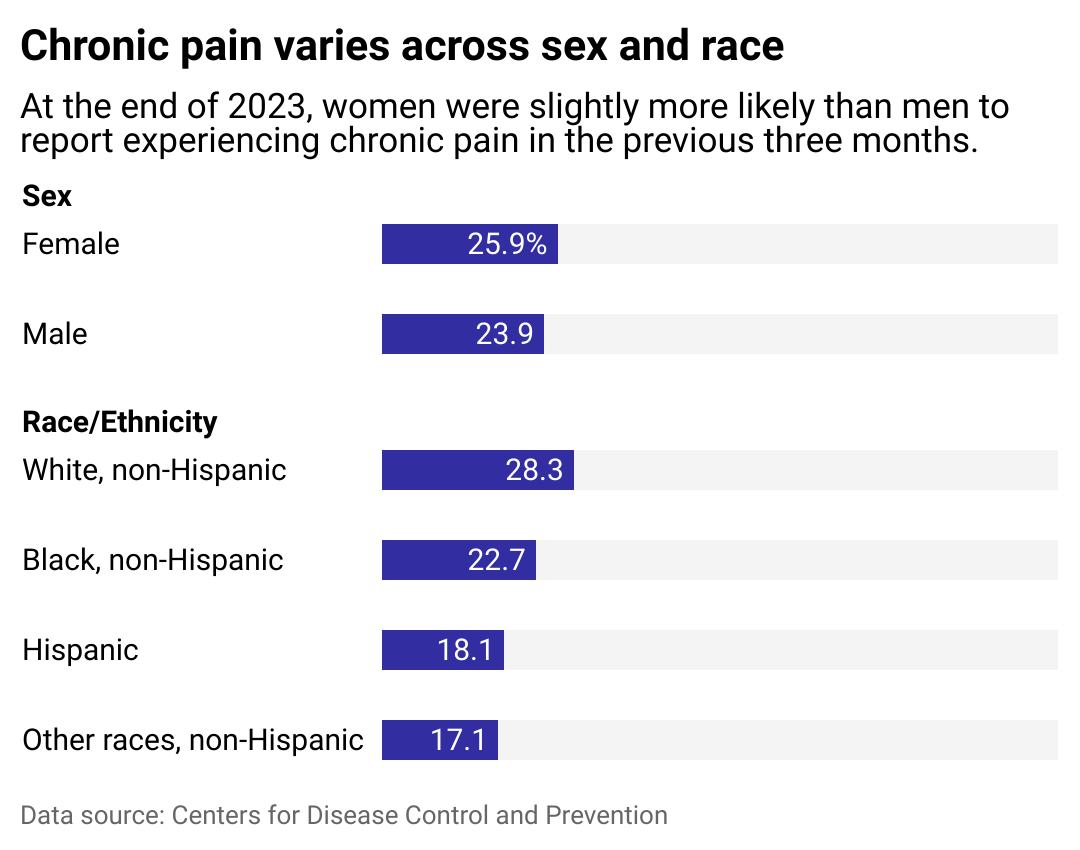
Medical professionals still have a lot to learn about the causes of chronic pain, but data does show that it affects more women than men and that the number of people who say they experience the condition is increasing.
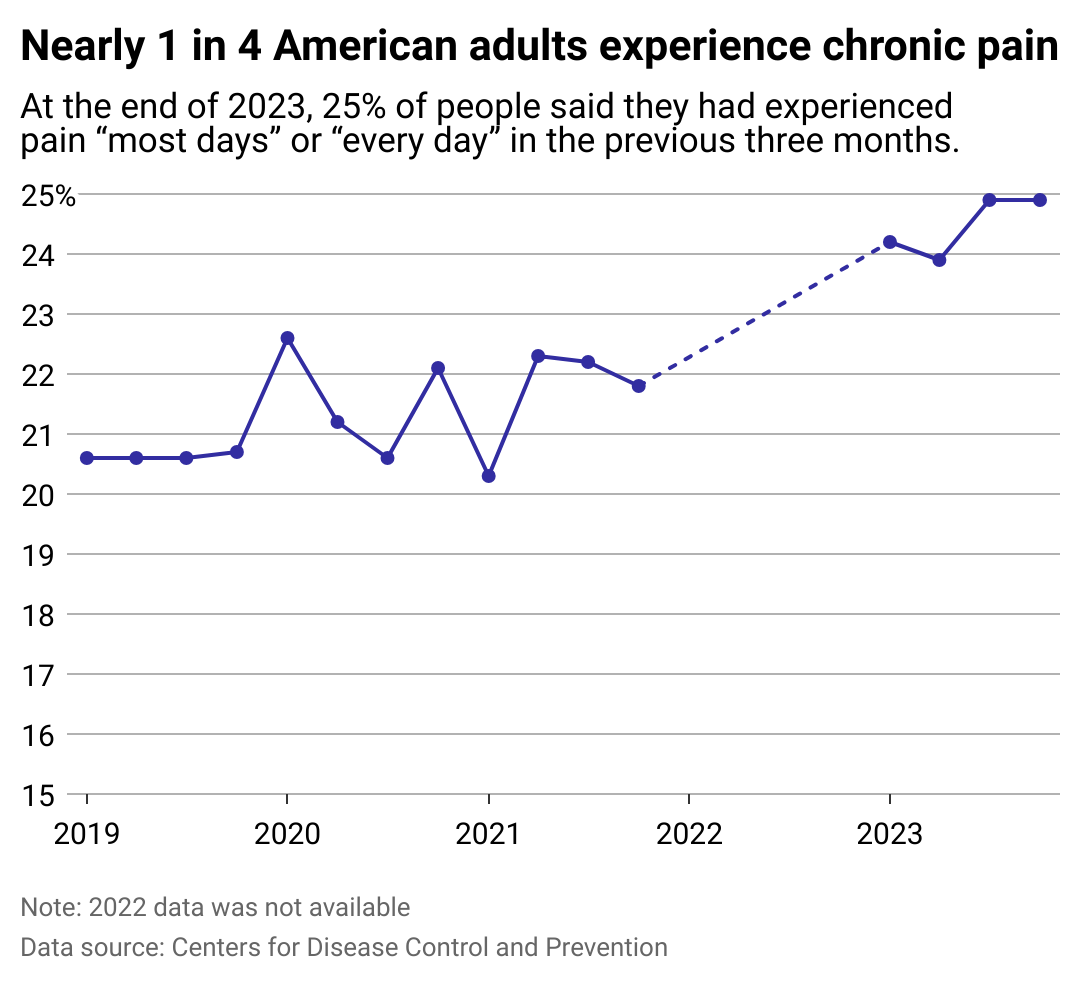
More Americans seeking help for chronic pain
Chronic pain can be caused by a variety of factors, Jianguo Cheng, medical director of the Cleveland Clinic Consortium for Pain in Ohio, told the medical news site Medscape. He described the phenomena of pain as a "complex mix of genetic, biological, and psychosocial dimensions that can cause ongoing pain out of proportion to the original limited injury that triggered it."
Martin Cheatle, director of behavioral medicine at Penn Pain Medicine Center, also told the medical news outlet that an aging population, obesity, and lifestyles characterized by inactivity have all contributed to an increase in chronic pain, which requires a comprehensive approach to care.
More recently, there has been a push to treat pain using approaches that take into account the physical, mental, and social aspects of chronic pain. Chronic pain is often associated with anxiety and depression, not only because of its impact on a person's quality of life, but because these conditions tend to be interconnected and processed in the same regions of the brain as pain processing and emotional regulation.
There has been little innovation in alternative pain treatments over the past two decades, as American health care providers overly relied on opioids for patient care, leading to a devastating public health crisis. Health insurance does not always meet the needs of patients with chronic pain, either—partially because it is difficult to quantify the intensity and duration of pain. Doctors tend to use a pain scale of 0 to 10, but this rating system is not always comprehensive. It can lead to over- or under-prescribing medicine depending on an individual's description or tolerance for pain. Complementary approaches, such as mental health support, are not always covered by health insurance.
Since existing medications rarely alleviate pain completely, there is more emphasis in the field to treat the condition with multidisciplinary treatments. Patients can benefit from nerve block treatments and spinal cord stimulation or learn self-managed pain relief skills aimed at helping diminish pain in the mind and body. Keeping the body active and healthy sleep patterns can also significantly impact pain symptoms and encourage resilience.
Some groups more likely to experience chronic pain
Many Americans are going without the effective pain treatment they need for a plethora of reasons. Access to specialists is one critical reason: Only 8% of people live in areas served by pain care specialists, researchers at Boston University found in a review of studies published between 2000 and 2024. In rural areas, compounding factors such as working in physically demanding jobs, a shortage of health care providers, and higher poverty and uninsured rates, make getting pain relief more challenging than in urban areas.
Recent progress in nonpharmacological interventions to alleviate chronic pain has put alternative forms of treatment on the map. Heat therapy and cryotherapy, massage therapy, cognitive behavioral therapy, and low-level electrical stimulation known as TENs have all been shown to reduce chronic pain, according to a 2023 article in the BMC Medicine journal. However, the efficacy of these and other noninvasive therapies depends on various factors, including the location and intensity of pain. While they may be used to supplement other treatments, further research may be needed.
How pain is treated may also differ depending on who is reporting it. Although women and girls are more likely to experience chronic pain than men, their pain is often overlooked, impacting their access to treatment. The term "medical gaslighting" emerged recently when videos of women describing the intense pain of IUD insertion went viral. The CDC provided new clinical guidelines to manage IUD insertion pain, but some physicians say that pain management options are still limited. The problem is compounded by a lack of clinical research on pain during gynecological procedures.
Black, Hispanic, and Native people, who already experience disparities in health care, are less likely to receive adequate pain management than white people experiencing chronic pain.
American Indian and Alaska Native people are twice as likely to report chronic pain when compared to Asian non-Hispanic and Hispanic adults, according to CDC 2023 data. When seeking help for persistent, disabling pain, Black men are less likely than white men to receive treatment or pain relief.
Racial and gender bias add multiple barriers to access pain treatment for Black women. A 2022 study in Reproductive Science found that biases toward Black women prevented or delayed endometriosis diagnosis, making them 50% less likely to be diagnosed with this painful condition, which already causes suffering in many women for 4 to 11 years before diagnosis.
Chronic or high-impact chronic pain is also associated with groups of people who are unemployed, living in rural communities, experiencing poverty, are bisexual, on public health insurance, are veterans, or are divorced or separated, according to analysis in 2023 of CDC data by the U.S. Pain Foundation.
As medical professionals give prognoses and monitor the progression of chronic pain, an approach rooted in realistic optimism may provide a path forward. Dr. Cheng told Medscape, "I don't expect miracles in 10 years' time, but we're making rapid progress in understanding the genetics of chronic pain and the mechanisms of disease and therapy."
Story editing by Natasja Sheriff Wells. Copy editing by Sofía Jarrín.



