The hidden health crisis: How loneliness is making America sick
The hidden health crisis: How loneliness is making America sick
New research reveals loneliness correlates more strongly with physical symptoms than any other demographic factor, yet half of sufferers never discuss it with their doctor
Nearly one in three American adults often or always feel lonely, according to new research from Wysa that reveals loneliness isn't just a social problem; it's a clinical one with profound implications for both mental and physical health.
The comprehensive study, which surveyed 2,044 representative American adults in 2025, uncovers a striking correlation between persistent loneliness and a wide range of health symptoms including depression, chronic pain, fatigue, and insomnia. What makes this research particularly significant is its finding that loneliness relates to these common ailments more closely than any other demographic factor, including age, gender, employment status, or living situation.
A Generation Defined by Isolation
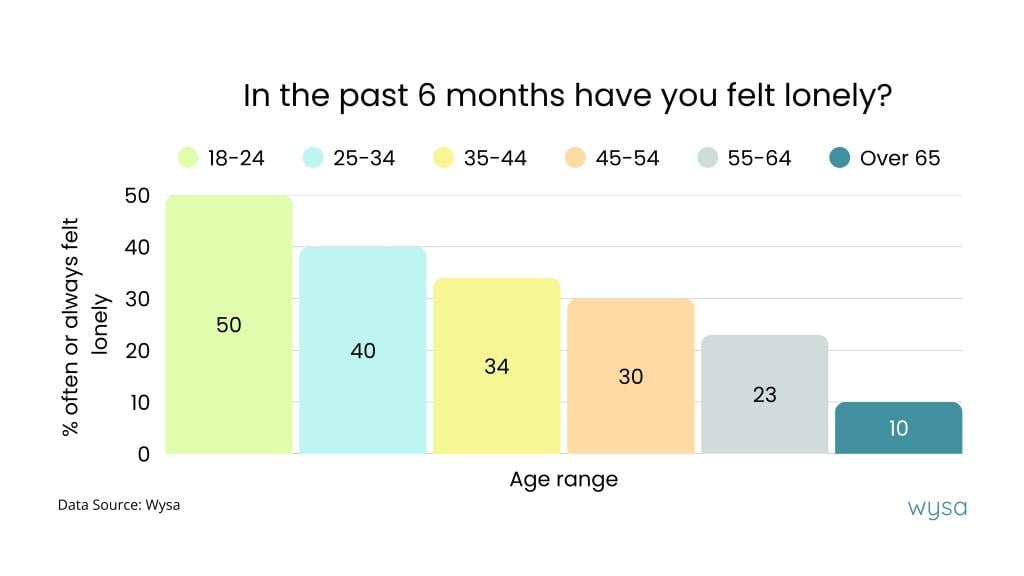
The data paints a sobering picture of modern American life, particularly for younger generations. Among adults aged 18 to 24, a staggering 50% report feeling lonely often or always, essentially half of young adults are experiencing persistent emotional isolation. This drops to 40% for those aged 25 to 34, and continues declining with age: 34% for 35- to 44-year-olds, 30% for 45- to 54-year-olds, 23% for 55- to 64-year-olds, and just 10% for those over 65.
The dramatic decline in loneliness with age hints at fundamentally different social experiences across generations. For today's youngest adults, loneliness appears to be a defining characteristic of early adulthood, likely influenced by pandemic disruptions, digital communication replacing face-to-face interaction, and evolving social structures.
Interestingly, men and women experience loneliness in roughly equal measure, challenging assumptions that emotional isolation primarily affects one gender. The research found 29% of men and 32% of women suffer from frequent loneliness, a negligible difference that underscores how universal this challenge has become.
Living Together, Feeling Alone
Perhaps the most surprising finding challenges our fundamental assumptions about what causes loneliness. Half of adults living with their parents report feeling lonely often or always. Similarly, one in 2.8 adults living in shared housing with other adults experience persistent loneliness. One in three single parents and one in three people living alone report frequent loneliness.
By contrast, only one in five adults living with a partner feel this way regularly.
This data overturns the common belief that isolation equals solitude. Loneliness, the research makes clear, is about the absence of meaningful connection and can thrive just as easily in crowded rooms as in empty homes. Simply sharing physical space with others provides no guarantee against emotional disconnection.
The Mind-Body Connection Americans Already Recognize
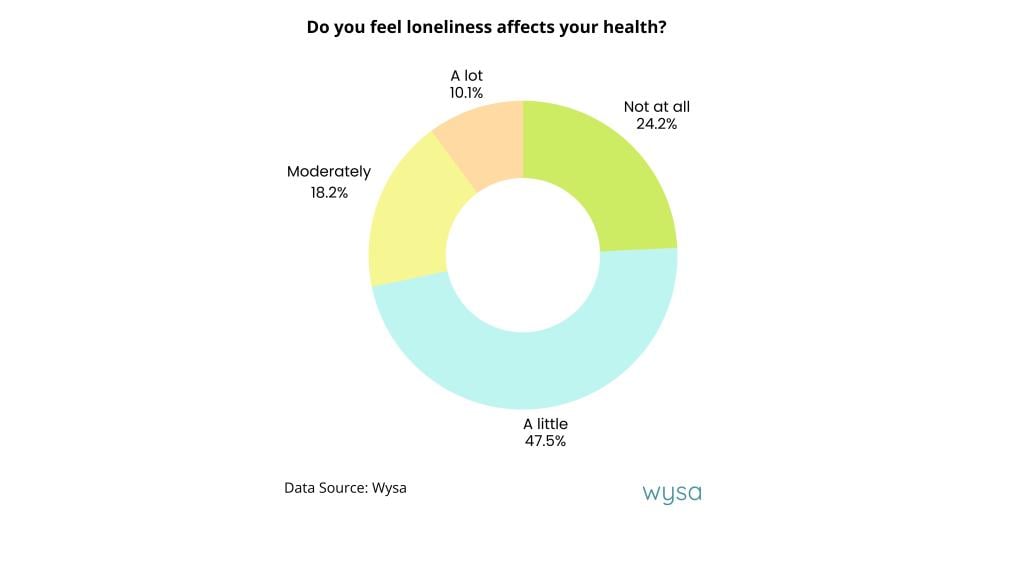
Americans themselves already understand that loneliness affects their health. When asked directly, nearly half acknowledged that loneliness impacts their well-being at least a little, with 10% saying it affects them "a lot."
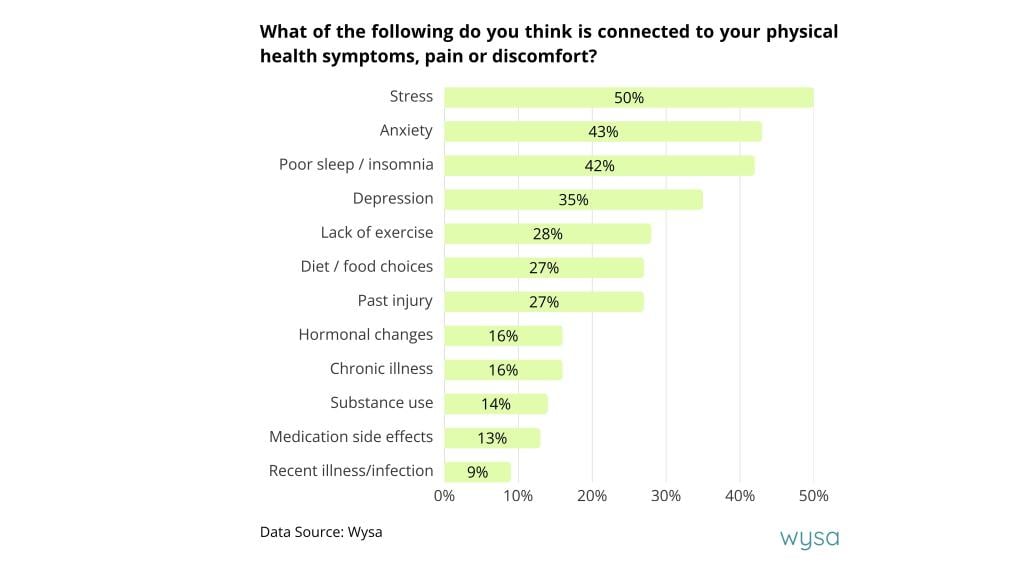
More tellingly, when asked what factors they believe contribute to their physical health symptoms, pain, or discomfort, Americans overwhelmingly pointed to mental health states rather than physical causes. Fifty% cited stress, 43% blamed anxiety, 42% identified poor sleep or insomnia, and 35% pointed to depression. By comparison, far fewer attributed their physical symptoms to lack of exercise (28%), diet or food choices (27%), past injury (27%), or hormonal changes (16%).
People instinctively understand that their physical symptoms connect to their mental well-being. Yet healthcare systems continue to treat mind and body separately, creating a disconnect between patient intuition and medical practice.
The Devastating Physical Toll
The research reveals just how accurate these patient instincts are. Among those who feel lonely often or always, an alarming 79% report experiencing moderate to severe pain or physical discomfort most days. This compares to just 41% of those who rarely or never feel lonely, nearly double the rate.
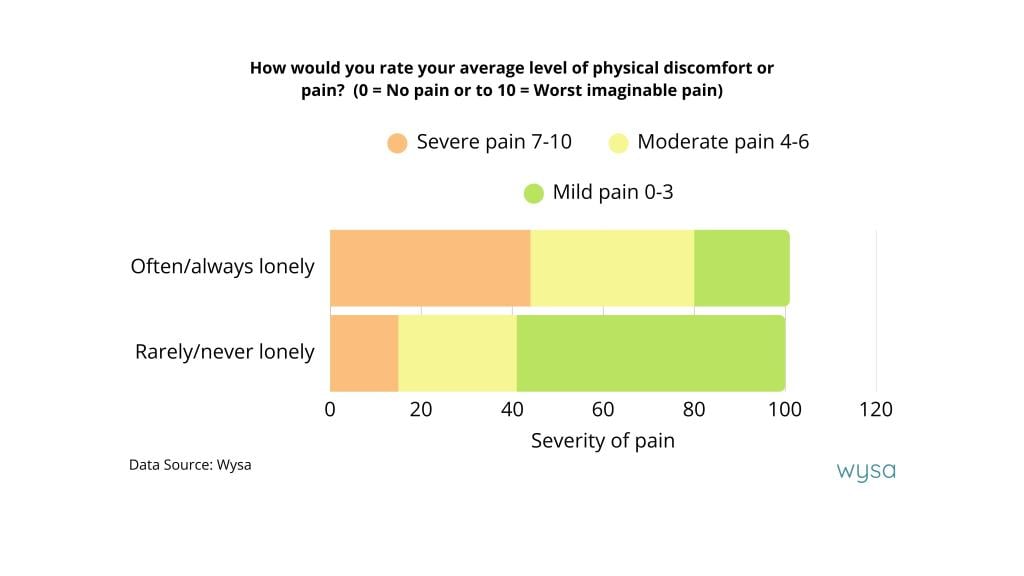
The correlation with severe pain is even more dramatic. Forty-four percent of frequently lonely individuals report severe pain levels (7 to 10 on a pain scale), compared to only 15% of those rarely lonely.
Sleep disturbances tell a similar story. Fifty-eight percent of frequently lonely people report trouble sleeping often or always, compared to 15% of those rarely lonely. Fatigue follows the same pattern: 52% versus 15%.
The research also documented significant correlations between loneliness and other common symptoms seen in primary care settings. For headaches and migraines, 39% of frequently lonely individuals suffer often or always, compared to 8% of rarely lonely people. For digestive discomfort, the figures are 29% versus 6%.
Six in ten people who feel lonely most of the time also screened positive for depression, compared to just 7% of those who rarely or never feel lonely, a stark illustration of how emotional isolation and mental illness intertwine.
The Treatment Gap
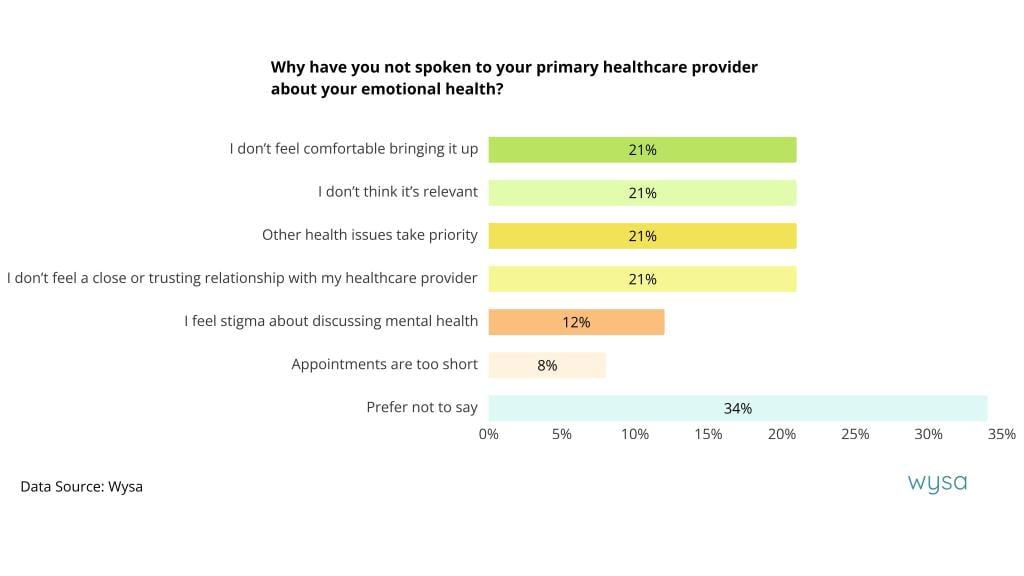
Despite this clear connection between loneliness and health, a troubling treatment gap persists. While half of Americans have discussed their emotional health with their primary care provider, the other half have not, and their reasons reveal systemic barriers in our healthcare approach.
Among those who haven't spoken to their doctor about emotional health, 21% said they don't feel comfortable bringing it up. Twenty-one percent also cited three other barriers: feeling it's not relevant, believing other health issues take priority, and lacking a close or trusting relationship with their provider.Another 12% feel stigma about discussing mental health. Finally, 8% said appointments are simply too short.
Even among the 43% who have tried accessing professional behavioral health support, only one in three found it easy to access. One third described it as somewhat easy, while the remainder found it neutral, somewhat difficult, or very difficult.
What Patients Want
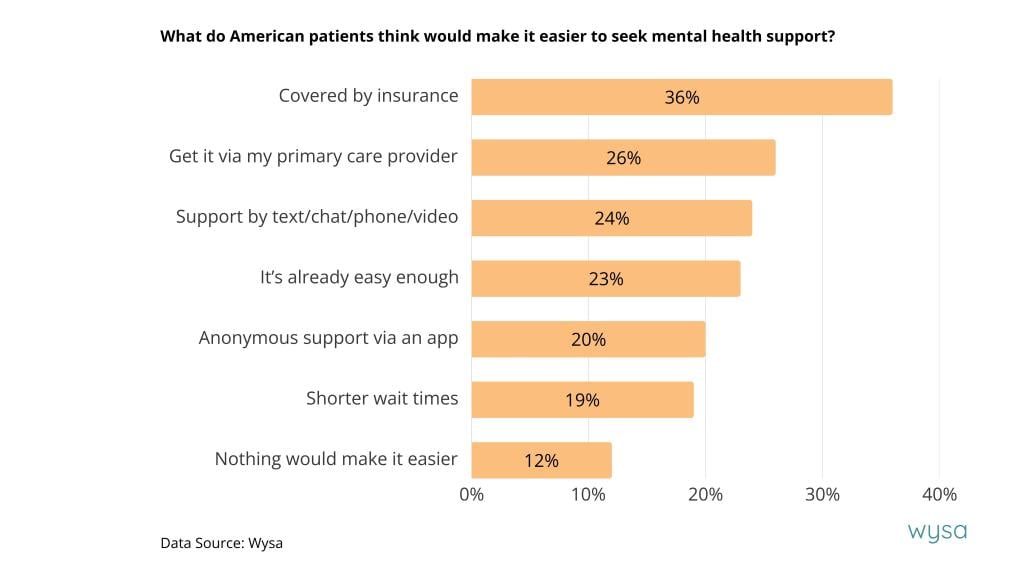
When asked what would make it easier to seek mental health support, the answers pointed toward clear solutions. Thirty-six percent of patients are simply unaware that insurance can cover mental health services, an information gap that could be addressed immediately. Twenty-six percent would like to access emotional support directly through their primary care provider. Twenty-four percent expressed interest in remote support via text, chat, phone, or video. Twenty percent would value anonymous support via an app, while 19% are discouraged by long wait times.
Notably, 23% said it's already easy enough, suggesting that for many, the barriers are less about availability and more about awareness, integration, and stigma reduction.
A Call for Integrated Care
This research arrives at a critical moment when healthcare delivery is increasingly moving to remote and digital platforms. While technology offers powerful tools for expanding access to care, the findings underscore that regular human contact remains the primary mechanism for ensuring meaningful healthcare relationships.
The solution lies not in choosing between human and digital care, but in embracing integrated, collaborative models that address both mental and physical health together. When patients already attribute their physical symptoms primarily to stress, anxiety, insomnia, and depression, treating these as separate from physical care makes little clinical sense.
Loneliness may feel personal and invisible, but its association with health challenges is clear and measurable. Like other complex public health issues, it requires a coordinated, human-centered response that bridges the gap between mental and physical healthcare. Only by recognizing loneliness as the clinical issue it is, not merely a social one, can we begin to address the suffering of millions of Americans whose health is deteriorating in plain sight, often in crowded rooms.
This story was produced by Wysa and reviewed and distributed by Stacker.