Answers to 30 common COVID-19 vaccine questions
Answers to 30 common COVID-19 vaccine questions
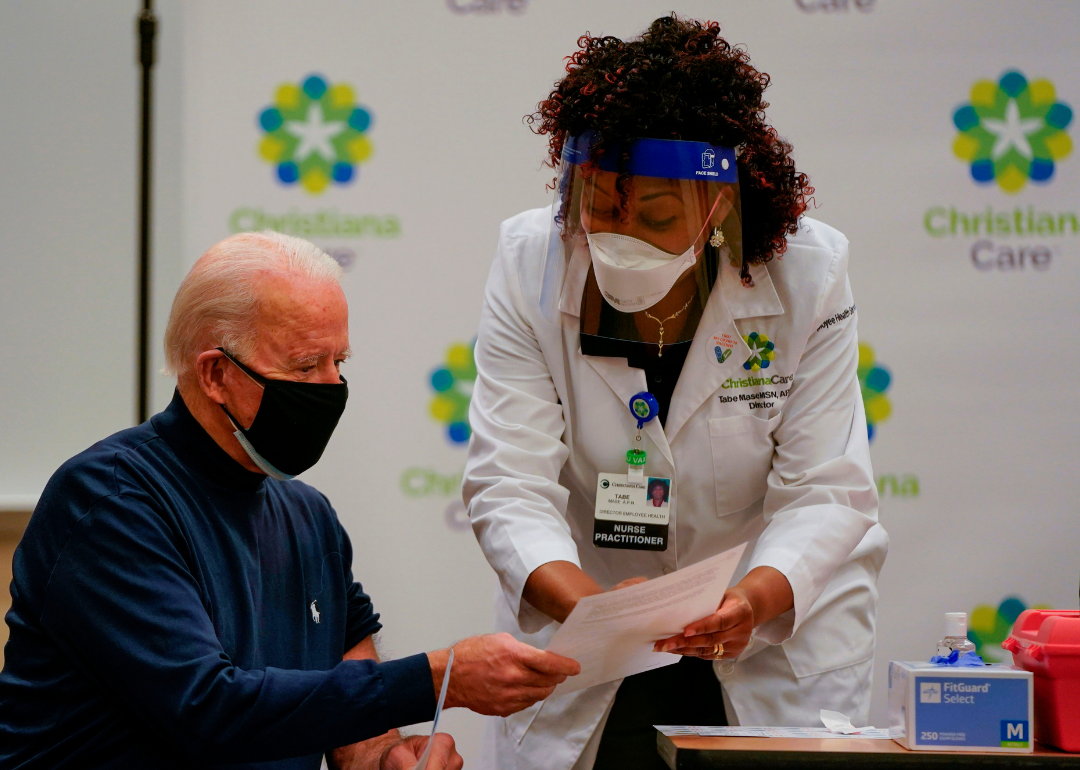
On Dec. 14, 2020, the United States began vaccinating people against the SARS-CoV-2 virus that causes the COVID-19 illness. The vaccine rollout has been very fast, as the virus was only identified for the first time in November 2019. While impressive, this speed has also left a lot of people with a lot of questions. The questions range from the practical—how will I get vaccinated?—to the scientific—how do these vaccines even work?
A successful vaccination campaign relies on a large enough group of people getting the vaccine in order to achieve what is known as herd immunity. While that exact number is still unknown, it is estimated the 80-90% of the population must be immune—either by vaccination or prior exposure to the virus—in order to achieve herd immunity. This means it's extremely important that people feel confident in the vaccines and vaccination process.
In order to help people better understand both, Stacker scoured news outlets and public health resources, especially the Centers for Disease Control's (CDC) COVID-19 vaccines FAQ site, to compile and answer 30 common questions about COVID-19 vaccines. This resource will explain how the vaccine works, when and how you should expect to receive yours, how it will be distributed, who should and shouldn't get the vaccine, when more vaccines will be available, and what to expect now that scientists are discovering new coronavirus mutations even as vaccinations are taking place.
While much is still unknown about the coronavirus and the future, what is known is that the currently available vaccines have gone through all three trial phases and are safe and effective. It will be necessary for as many Americans as possible to be vaccinated in order to finally return to some level of pre-pandemic normalcy, and hopefully these 30 answers provided here will help readers get vaccinated as soon they are able.
Understanding COVID-19 with Stacker:
From Wuhan to the White House: A timeline of COVID-19's spread
How vaccines get made and approved in the US
15 ways doctors are now treating COVID-19
27 factors that make you vulnerable to COVID-19
35 COVID-19 symptoms to be aware of
How do the Pfizer and Moderna vaccines work?
The Pfizer and Moderna vaccines are both mRNA (messenger RNA) vaccines. These are a new type of vaccines that trigger an immune response by using mRNA to instruct cells to make a harmless snippet of the spike protein that is found on the surface of the Sars-CoV-2 virus, which causes COVID-19. This protein triggers an immune response in the body, producing antibodies and protecting vaccinated people from getting infected if they are exposed to the real virus.
How do the two approved vaccines differ?
While the Pfizer and Moderna vaccines are both mRNA vaccines with similar efficacy (95% and 94.1% respectively), they have a few important differences. For one, while the Pfizer vaccine is approved for people 16 and older, the Moderna vaccine is restricted to those 18 and older. And while both need two doses, the Pfizer one requires 21 days between doses and Moderna requires 28. A key difference, however, is storage temperature. The Moderna vaccine is easier to ship, because it needs to be stored at -4 Fahrenheit. On the other hand, the Pfizer vaccine needs to be stored at a much lower temperature: -94 Fahrenheit.
Are there any side effects?
Both the Pfizer and Moderna vaccines can trigger a range of side effects. Most are mild, such as pain at the injection site, headache, fatigue, and muscle and joint pain, and some people in clinical trials reported fever. These side effects are completely normal and are a symptom of the immune response kicking in. However, there have been very few more serious allergic reactions to the Pfizer vaccine.
How did we develop vaccines so quickly?
These vaccines were able to be developed so quickly because the U.S. Congress directed nearly $10 billion to Operation Warp Speed, which was the project with the goal of producing and delivering 300 million safe and effective doses of vaccine by January 2021. While that goal has not been met, the vaccines were developed unprecedentedly quickly. On Twitter, Dr. Sydnee McElroy, a family doctor, compared the speed of vaccine development to expedited shipping, where you pay more to get your items faster, but they are still handled safely.
How do we know these vaccines are safe?
These vaccines were approved in record time through emergency use authorization. However, they still went through all three phases of clinical trials in order to ensure safety and efficacy. In addition, the vaccine went through a manufacturing investigation and has been approved by the FDA. And as the vaccine is rolled out, it is monitored for any unexpected side effects.
What does 'emergency use' mean vs. full approval?
As previously stated, the Pfizer and Moderna vaccines have been authorized for emergency use, signalling how dire the pandemic is. However, this does not mean that the vaccine has been approved by the FDA. The process for approval “involves rigorous reviews of all available data on the product and can take several months.”
Why are two doses necessary?
By giving multiple doses of a vaccine, the body has a chance to produce more antibodies against the virus because it is exposed to more antigens, which create more memory cells. This means that when the body is exposed to the real virus, it will have a faster and more effective antibody response. In the case of these two vaccines, two doses is the best way to create the most effective number of memory cells and antibodies.
How long does it take for the vaccine to work?
The Pfizer vaccine offers immunity no less than seven days after the final dose and the Moderna vaccine offers immunity no less than 14 days after the final dose. It is so far unknown how long immunity will last, although experts think that it should last for a few years. However, more studies will need to be done.
Should I get the vaccine if I'm pregnant or breastfeeding?
The vaccine was not tested on pregnant or breastfeeding people. However, the Food and Drug Administration will allow them to opt for immunization against the virus if they choose. In a New York Times article, Emily Wilson, an obstetrician working at Northwestern University and a member of the COVID-19 task force of the Society for Maternal and Fetal Medicine, said, “This is a really huge step forward in recognizing women’s autonomy to make decisions about their own health care.”
Why have some people had allergic reactions?
In very few instances, the Pfizer vaccine has caused a severe allergic reaction. Scientists think this might be due to a compound, polyethylene glycol (PEG), used to package the mRNA. PEG has never been used in an approved vaccine (this is an authorized vaccine), but it is found in drugs that occasionally trigger severe anaphylactic reactions. However, some scientists are still skeptical of the causation.
Should I get the vaccine if I carry an EpiPen?
The CDC recommends that people with a history of severe allergic reactions should still get vaccinated, as long as their allergic reactions are not related to vaccines or injectable medicines. However, people allergic to polyethylene glycol (PEG) or polysorbate should not get the vaccine.
Are COVID-19 vaccines safe for kids?
The current Pfizer and Moderna vaccines are only available to teenagers 16 and 18 years old, respectively. Because children’s immune systems are different from adults and respond differently at different ages, research that’s been done on the vaccines for ages 16 and up needs to be repeated on children of younger ages. However, a full pediatric vaccine will hopefully be available by late 2021. And luckily, the virus so far seems to impact children much less seriously than adults.
What is a ‘first priority’ group and who is in it?
In order to prioritize who will be vaccinated first and in what order, the CDC’s Advisory Committee on Immunization Practices (ACIP) has recommended that the first priority group include healthcare workers and long-term care residents, for example those in nursing homes. This priority group is estimated to consist of around 17.6 million people.
When will I get vaccinated?
When a person will get vaccinated depends on their age, health condition, profession, and where they live. After the first priority group is vaccinated, the next group will be essential non-healthcare workers and people 75 and older. However, states have the final say, so it may not be exactly the same across the country.
What are the priority health conditions for vaccination?
The ACIP says that the following high-risk health factors would qualify someone to be part of a priority group for the vaccine: "obesity, severe obesity, type 2 diabetes, COPD, a heart condition, chronic kidney disease, cancer, immunocompromised state as the result of a solid organ transplant, sickle cell disease, pregnancy, and smoking."
Which jobs are included in top priority essential workers?
Essential workers are defined as those whose jobs cannot be done from home and whose jobs are necessary for a functioning society. Because of this, they will be in a priority group for vaccination. Essential workers include: first responders (firefighters, police), teachers and educational support staff, food and agricultural workers, manufacturers, correctional workers, U.S. Postal Service workers, public transit workers, and grocery store workers.
Is there an alert system to tell me when I can be vaccinated?
Because vaccine distribution has been left up to the states, the best answer to this question would be found on your local public health agency website or with your primary care physician. Some states, such as New York, are planning to create a website where you can check your eligibility, and others, such as Maryland, will allow residents to preregister for the vaccine via their state's existing immunization information system. On the other hand, some counties in Florida and Oklahoma are using online RSVP systems such as EventBrite and SignUpGenius—usually used for parties and events—to sign people up.
How are doses allocated to states?
According to an NPR article from November 2020, the government chose to allocate the first shipments of coronavirus vaccines based on population. This ignored a CDC proposal to distribute them instead based on high-risk groups.
How does dose distribution work?
Distribution of the vaccine started 24 hours after the first Emergency Use Authorization. Each week on Tuesdays, allocation lists are made available to states and jurisdictions to order from. Shipments then take place the following Monday. These orders won’t necessarily arrive all at once, but throughout the week. Sites get delivery notifications from private shipping partners.
How are vaccinations being counted?
Because the vaccine rollout is so localized, the numbers of vaccinations are being tracked by a mix of interconnected state and federal databases. This will likely include over 100 data systems along with inventory management systems from Fed and UPS and data management systems from Walgreens and CVS. It will be difficult to coordinate all this data along with data from the vaccination sites.
How many people have been vaccinated so far?
The up-to-date numbers on COVID-19 vaccinations can be found on the CDC COVID Data Tracker website. As of Jan. 9, 2021, a total of 6,688,231 had received the first dose of one of the two vaccines, and 22,137,350 doses had been distributed.
Where will I be able to get vaccinated?
Vaccines are being administered through doctors, pharmacies, health centers, state and local health departments, and travel clinics. As previously mentioned, vaccinations are being handled locally and this information varies from place to place, so for the most accurate and personalized information, visit vaccines.gov—the website from the Department of Health and Human Services—or your local health department’s website.
How much does it cost to get vaccinated?
According to the CDC, vaccine doses purchased by the federal government are available at no cost. However, vaccine providers may charge an administrative fee for giving the shot. This fee can be reimbursed by the patient’s insurance company.
Do I need to provide personal information?
While this answer may vary somewhat by state and county, the CDC will collect personal information such as names, addresses, ethnicities, and birthdays of recipients of the COVID-19 vaccine. They are asking states to sign a data sharing agreement to hand over data taken at vaccination sites to the federal government. Administration officials say that the data won’t be shared with other federal agencies, rather that it is needed to track adverse reactions and effectiveness.
How far apart are the first and second doses?
In order to be as effective against COVID-19 as possible, both the Pfizer and Moderna vaccines require two doses. The Pfizer vaccine requires an interval of 21 days between doses, and the Moderna vaccine an interval of 28 days.
Do we still need masks and social distancing after vaccination?
Even after receiving two doses of the COVID-19 vaccine, it will still be necessary to wear a mask and follow the other recommended hygiene and distancing protocols. This is because it will take time for everyone to be vaccinated and because, according to the CDC, “experts need to understand more about the protection that COVID-19 vaccines provide before deciding to change recommendations on steps everyone should take to slow the spread of the virus that causes COVID-19.”
How does the new stimulus bill impact vaccinations?
The $900 billion coronavirus stimulus bill will allocate between $8 and $9 billion to vaccine distribution. This is at least $2 billion more than would have been provided under earlier proposals for the stimulus package.
How does the new coronavirus mutation affect current vaccines?
At the end of 2020, two new coronavirus mutations were identified from South Africa and the United Kingdom. As of Jan. 8, 2021, a study showed that the Pfizer vaccine would still be effective against these mutations. However, as these mutations are new, scientists are still learning about them. In addition, as the virus continues to spread, new mutations may occur, and scientists do not know how they will respond to the vaccine.
Why did the UK change its dosing strategy?
The U.K. has decided to prioritize getting people their first doses of the vaccines before giving people the second doses. This means that people could wait up to 12 weeks between doses. They have chosen to do this because numbers of positive cases are rising sharply and, according to U.K. officials, “At this stage of the pandemic, prioritizing the first doses of vaccine for as many people as possible on the priority list will protect the greatest number of at risk people overall in the shortest possible time.” Scientists are split on whether this is a good strategy.
What other vaccines are in the pipeline?
There are a large number of other vaccines in the pipeline. Along with the Pfizer and Moderna vaccines, there is an AstraZeneca vaccine, which has been approved in some countries such as the U.K. and India. There are seven other vaccines in early or limited use, 20 in Phase 3 trials, 20 in Phase 2 trials, and 40 in Phase 1 trials.



